Leaderboard
-
Points8,944Posts
-
.jpg.c873029d6ea548a78cb17a21407a1303.jpg) Points2,989Posts
Points2,989Posts -
-
Points1,580Posts
Popular Content
Showing content with the highest reputation since 06/28/2007 in all areas
-
Gold Medal.
Gold Medal.
Ally and 36 others reacted to Malcolm Needs for a post in a topic
37 pointsI am enormously honoured to announce that I am going to be awarded the Gold Medal of the British Blood Transfusion Society at their Annual Scientific Meeting in Brighton this year. It is awarded to an individual for their exceptional and long standing services to the Society and to the practice of blood transfusion in the UK. Sorry if this sounds egocentric, but I am very excited.37 points -
Ruling out Kell with Heterozygous cells?
Ruling out Kell with Heterozygous cells?
Andrea Pointer and 28 others reacted to Malcolm Needs for a post in a topic
29 pointsI am going to be REALLY unpopular here, but I'm going to say it anyway (because I am a pedant)!!!!!!!!!!! Antigens CANNOT be either heterozygous or homozygous; only genes can be heterozygous or homozygous. An antigen can be described as either showing homozygous expression, or heterozygous expression. That having been said, is a red cell sample that types as K+k- phenotypically, genotypically K/K or K/Ko, or even K/k, with a mutation within the Kell gene that prevents the k antigen being expressed and detected with all anti-k grouping reagents (just in case anyone doesn't believe me - we had one!). That's got that off my chest. Now then, there is NO doubt that there are some anti-K's around that only react with K+k- red cells (dosage), but they are fairly rare, however, how many people use antibody screening red cells that are K+k-? I doubt if there are any. Therefore, we are all ruling out anti-K using red cells with apparent K antigen heterozygous expression on every single sample that (apparently) has no atypical alloantibodies present. Am I wrong about this? It follows, therefore, that, over the years, there MUST have been occasions when a patient with a very weak anti-K (one that is only detected using red cells that are apparently showing homozygous expression) and who has been transfused with K+ blood (do the maths). As far as I know, there are no papers within the literature that report a case of either a delayed or an acute transfusion reaction as a result of this. Yes, this may cause the anti-K to become stronger (and, hence, be detectable using an apparent heterozygous red cell sample showing K+k+ expression), but then, if this happens, you give K- blood. So, my considered answer is that you can exclude using K+k+ red cells. I shall now go and lie down!!!!!!!!!!!!!29 points -
I'm coming back to Providence!
I'm coming back to Providence!
Walter Isenheim and 20 others reacted to Malcolm Needs for a post in a topic
21 pointsThanks to a very generous invitation from the organisers (in particular Phil Hoffman, aka Dr Pepper on this site, and Maddie Josephs, Chair) I will be attending and speaking at the 69th Annual Clinical Laboratory Science Convention - Central New England (ASCLS - CNE) taking place at the Rhode Island Convention Center between May 9th and May 11th 2017. I will be talking on Wednesday 10th May 2017, giving a lecture entitled, "An In Depth Description of the Kell Blood Group System." and then, after a well-deserved break for the delegates, and for those that can stand it, a second lecture entitled, "King Henry Viii, McLeod Syndrome, Chronic Granulomatous Disease and Kx." Sorry if this comes across as being "big headed", but I am really excited about coming back over to the USA.21 points -
Mock-up cases
Mock-up cases
ElinF and 19 others reacted to Bb_in_the_rain for a post in a topic
20 pointsFor those of who works in transfusion service laboratory and would like to learn more reference cases, I can post some mock-up cases here. If you would like me to do it, please hit the "heart" button on this post. If enough folks want to practice case studies on reference lab cases, I can post mock-up cases here weekly or so..20 points -
31/10/16.
31/10/16.
Gnapplec and 18 others reacted to Malcolm Needs for a post in a topic
19 pointsWell, that's me finished. I am officially retired from work - but not from this wonderful site!19 points -
Issuing Units and "Contamination"
Issuing Units and "Contamination"
KKidd and 18 others reacted to Malcolm Needs for a post in a topic
19 pointsYou could always irradiate the blood bag (as well as the blood), while the stupid nurse is holding it!!!19 points -
Storage of non-blood products in BB fridge
Storage of non-blood products in BB fridge
melvolny and 17 others reacted to Malcolm Needs for a post in a topic
18 pointsI'm afraid that may not work. We used to keep all of our "in-date" antisera on the top shelf, and our out-dated teaching antisera on the bottom shelf. This meant that, if any of our "in-date" antisera fell off the shelf into the out-dated teaching antisera, and we didn't notice, it didn't matter. Sadly, what I had not taken into account was the fact that one of our inspectors (I can't remember whether it was CPA or MHRA) knew much more about physics than did I, and explained to me, in huge detail, that the out-dated antisera must be kept in a separate fridge, in case the out-dated teaching antisera defied the Law of Gravity and flew up to the top shelf and secreted themselves there. So, everyone out there, be aware that the Physical Laws DO NOT APPLY to out-dated antisera, which is pretty dangerous when you think about it. In fact, I now rarely open the door of the fridge that contains our out-dated teaching, for fear of flying bottles, and NEVER without holding a stout stick, just in case!18 points -
Storing Saline Cubes
Storing Saline Cubes
jshepherd and 16 others reacted to John C. Staley for a post in a topic
17 pointsI'm going to be blunt. This is ridiculous!! You have the potential of causing far more problems by removing the cubes from their protective container.17 points -
Positive Autocontrol in gel, negative DAT
Positive Autocontrol in gel, negative DAT
Ensis01 and 15 others reacted to Joanne P. Scannell for a post in a topic
16 pointsI composed an answer to this yesterday and must have gotten 'sideswiped' before I posted it! Anyway, here's what I have to add to this conversation ... You cannot compare gel to tube testing. Aside from the 'sensitivity' issue (DAT could be positive in gel, negative in tube), gel has a totally different premise that needs to be taken into consideration. Gel: Slippery RBCs will make it all the way to the bottom of the gel column during a given period of time at a given centrifugal force.Tube: Cells must be agglutinated.1. Therefore, gel results are affected not only by coating of RBCs with antibodies, but also coating (roughening) with just about anything (proteins, medications). In addition, changes in shape (e.g. sickling, acanthrocytosis, fragmentation) will cause a slower migration to the bottom. 2. You cannot expect an auto control to give the same results as a DAT because the autocontrol has plasma in it. (It's like all ladies are women but not all women are ladies.) Certain properties of the plasma will affect this downward migration (e.g. artifact, fibrin, TP ratio leading to rouleaux, cold agglutinins). 3. You cannot even expect the same 'DAT grade' with an auto vs DAT. The autocontrol contains the same enhancement medium as the tests. The presence of an enhancement medium will, ummm, enhance the antigen-antibody reaction. Suggestion: Don't mix your media. If Auto Control is positive in gel, don't bother running DAT with tube method; run it using same method as the Auto Control (gel) and be sure to include a 'negative' control using a buffer card with patient's cells. If the buffer control is positive: You cannot determine if DAT is pos or neg because the 'positive result' may be due to steric interferrence rather than 'coated with antibody'; check hemo smear for sickling, acanthrocytes, etc.If the gel DAT is positive and the control is negative, your patient cells have a positive DAT.If the gel DAT is negative, the positive auto could be a result of plasma abnormalities, check protein analysis, cold agglutin, etc.Hope I haven't overstayed my welcome ...16 points -
QC on Panels
QC on Panels
lehooke and 14 others reacted to John C. Staley for a post in a topic
15 pointsI have never qc'd panels and will be ending my career with that same statement, mostly, because at my current and final employer we don't perform antibody id's. This discussion is not a new one and will continue to pop up with new inspectors and new interpretations of old rules. Frankly, there is not anyway to realistically QC a panel and have confidence that the every antigen listed is detectable. Frankly I am surprised at the number of folks responding that they do some form of panel QC. In my ever so humble opinion you are providing nothing but smoke and mirrors to pacify some inspector. I suppose that as long as you are successful at this it's worth the effort.15 points -
Confused about dosage
Confused about dosage
BldBnker and 13 others reacted to SMILLER for a post in a topic
14 pointsFrom the My Two Cents Dept... I would just point out that it is important that people doing testing understand what and why they are doing what they are doing. I guess this goes without saying. I am not a fan of throwing computer AI at problems when staff have trouble understanding what it is they are doing. I get it that with staff shortages and what not, that generalists have a lot of hats to wear, but a computer algorithm should never be a substitute for appropriate education and regular, effective performance evaluation. Scott14 points -
He got the question right
He got the question right
tburl and 13 others reacted to Dr. Pepper for a post in a topic
14 pointsI have a not-serious question on each of my med tech student quizzes. I thought I'd share a current student's response to "Describe in 80,000 words or less why immunohematology is by far the most interesting department in the lab." I usually get charming BS like "Because Phil is awesome!", but this guy got a little deeper: "While not as engaging as Micro, Immuno, Heme or Molecular on the surface, Immunohematology (aka blood bank) is much more mentally taxing. It requires one to think through a process logically, using the tools at one's disposal in the metaphorical tool box, to produce a resulting reaction one can use to reason an answer to a medically potentially dangerous situation. On a theoretical level, this requirement leads to the utilization of the full extent of one's mental capacity, causing it to be psychologically fulfilling, and therefore the superior department of choice for the intellectual medical lab scientist. Also, the word agglutination is funny."14 points -
e and C titer
e and C titer
Ensis01 and 12 others reacted to Malcolm Needs for a post in a topic
13 pointsThe thing is tkakin, that most examples of anti-C (anti-Rh2) are not; they are actually anti-Ce (anti-Rh7)! This is largely because almost every red cell that causes immunisation against the C antigen expresses both the C and e antigens as a result of having the RHCe gene, rather than both the C and e antigens as a result of having both the RHCE gene and the RHce gene (which is why both the DCE and dCE haplotypes are so rare). On the other hand, monospecific anti-e is comparatively common. So, your lady's plasma is more likely to contain anti-Ce and anti-e, rather than anti-C and anti-e. As a result, if, as yan xia suggests, you would undoubtedly adsorb out the anti-e, but you still would not know if the remaining antibody specificity is anti-C or anti-Ce (or, of course, a combination of the two). Anyway, the specificity really doesn't matter. The point is that, as you suggest, the individual titres of what ever antibodies are present are totally irrelevant. Normally, an antibody, such as anti-C (or anti-Ce) or anti-e, are not going to cause clinically significant haemolytic disease of the foetus and newborn, until the titre reaches 32, and it really doesn't matter whether the specificity of the antibody is anti-C, anti-Ce or anti-e. Your Pathologist should explain this to your OB doctor to get him or her off your back (actually, to be honest, your OB doctor should already know this, but hey, life ain't always like that!).13 points -
Training new employees
Training new employees
Arno and 12 others reacted to Malcolm Needs for a post in a topic
13 pointsI would agree with mollyredone, but would go further, Not only do you need to record everything you say to him (and get him to counter-sign the record), you need to record everything you tell your own seniors, and get THEM to counter-sign what you have told them. THIS PERSON IS DANGEROUS. You, as a conscientious employee, should not have to take responsibility for this person, but, if the worst happens (and it well could), you want to make certain that you are not held responsible in law, but that the finger is pointed in the right direction. If you get your own seniors to counter-sign your written concerns, you will, not only be protecting your own future, but will also cause them sleepless nights until they do something about the situation.13 points -
On call phone calls
On call phone calls
jnadeau and 12 others reacted to tbostock for a post in a topic
13 pointsI'm on call 24/7. I tell them to consult the policy first. If you try and can't find it anywhere in a policy, ask your coworkers to show you where to find the answer. If nobody else on your shift can point you to it, THEN you call me. Do not guess! I get a lot more text messages than I do phone calls. Usually they already know the answer, they are just wanting me to confirm their answer. We have quite a few generalists on my eve and night shifts that are not very experienced with difficult BB issues, so I have no problem with them calling me. I would much rather that than a patient gets hurt. I feel like it's part of my job as BB Manager to support them and have them feel confident in asking for help when they need it. I think the key to "weaning" them from calling too much is giving them really great policies (written very simply so anyone can follow them, even if they have not done the test for a while) and some good flowsheets (which I am still working on) for antibody workups, RhIg workups, etc.13 points -
RHIG for pt receiving O pos RBC's
RHIG for pt receiving O pos RBC's
Ensis01 and 12 others reacted to John C. Staley for a post in a topic
13 pointsBut Malcolm, there is a very subtle but important difference between what is "possible" and what is "realistic". Personally, I would say that going through an exchange transfusion simply to prevent the formation of anti-D is not reasonable but then I'm married to a nurse who has an anti-D along with an anti-K and an anti-S so my view may be a little jaded. Oh ya, the D was provided by the birth of our son. Our daughter was effected by it to the point of needing a double exchange transfusion which, I should mention, is not quite as dramatic in an infant as it is in an adult. The daughter is now 31 and has three children of her own. I relate this to remind folks that having an anti-D is not the automatic kiss of death. Ok, enough of my semiannual philosophical drivel.13 points -
Plasma Freezer Down: Better Process for Temp Storage of Frozen Products
Plasma Freezer Down: Better Process for Temp Storage of Frozen Products
wellspl and 11 others reacted to jayinsat for a post in a topic
12 pointsAll, I am about to blow your mind.... Our plasma freezer is down and so is our backup. The freezer will not get colder than -18 C. I was preparing to move all the products into boxes with dry ice until I had a conversation with my 87 year old dad, a retired blood banker from University of Chicago. He said to me, do not take the plasma out of the freezer and put it in boxes, PUT THE DRY ICE IN THE FREEZER, IT IS THE BEST STORAGE BOX YOU HAVE!!!! MIND=BLOWN!!!! I did that. Our freezer is currently reading -25.1C and getting colder. Furthermore, the probes in the freezer continually monitor the temp in the freezer so you don't have to record temps every 4 hours, the chart is doing that for you!!! Isn't that cool? That perfectly illustrates the difference between wisdom and knowledge there. I wish we could hire my dad. I just had to share this here. PS. Freezer is now at -26.4C.12 points -
Microscopic Examination
Microscopic Examination
lehooke1 and 11 others reacted to Malcolm Needs for a post in a topic
12 pointsMany years ago, Peter Issitt stated that microscopes should be banned from Transfusion Laboratories (I think it was in the orange edition of his book) except for such tests where cells are being counted (such as the Kleihauer). Many years after his wise words, I still follow his advice, and have not (yet) been involved in a missed weak antibody that has caused a clinically significant haemolytic transfusion reaction (43 years in the job), and many of those tests were performed in opaque tiles and then, as we "modernised", tube techniques.12 points -
saline expiration date
saline expiration date
mpmiola and 11 others reacted to JHH1999 for a post in a topic
12 pointsTypically expiration dates are established by the manufacturer. They perform stability testing for the duration of the assigned expiration date to support it with data. Data shows the product is capable of performing up until the claimed expiration date. It may continue to function they just do not have data to support it. This should be done to support any "reagent" made that is not at least qualified in some way each day of use. Assigning an expiration date based upon the shortest dated component is not very good science. The different ingredients could be compatible with each other or could have a negative impact to on another. From a pure scientific and quality aspect one would prepare a reagent and place it on a stability schedule and test it periodically for performance. This data is then used to support the use. Any assessor should accept this science. A simple analogy I like. If you made a cake today with milk that had a use by date of tomorrow does that mean the cake is not good after a day. Of course not, since it is now in a different form and could be stored in a different way.12 points -
antigen negative units for patients with autoantibodies?
antigen negative units for patients with autoantibodies?
RJL12 and 11 others reacted to Malcolm Needs for a post in a topic
12 pointsThe point about warm auto-antibodies, even the ones that look exactly like an auto-anti-M, an auto-anti-Jka or a specific Rh antibody, such as auto-anti-e, is that they all tend to be mimicking specificities, and so, in reality, you might be fooling yourself by giving antigen negative units to the patient, but you will not be fooling the patient's immune system, and so the chances are that, in most cases, the antigen negative transfused red cells will last no longer than the patient's own red cells. "Cold" auto-antibodies tend to have true specificities, but, even if you can find antigen negative units, the red cells will usually not last as long as the patient's own red cells, because the patient's own red cells are coated with C3dg, which gives them some protection from removal from the circulation, whereas the transfusion red cells have no such protection. I agree with your Reference Laboratory - which, considering that is my own background, may not come as a surprise to a lot of people!12 points -
On call phone calls
On call phone calls
John C. Staley and 11 others reacted to jalomahe for a post in a topic
12 pointsI'm the Lead Tech of my department and I have my phone number posted in the department so the techs can call if they have questions. I tell them I'd rather they call me and I solve their problem/question quickly (hopefully) instead of them either spending a lot of time dithering about it and delaying results/care or doing something incorrectly, especially in the LIS, and it taking me hours later to sort it out and make the corrections. Additionally I live close by and have told techs, especially on evenings/nights that if they have something come in that they are having trouble handling to call me: example trauma/massive with antibodies. Some techs are comfortable calling me so will be more likely to call, others not so much and won't call even when they should have. I am never upset with someone calling even if they wake me from a sound sleep because if they are unsure enough to call me I don't want them to hesitate because they think I might yell at them. If it's something that they should have known how to do or should be able to follow the procedure I take that up with them the next day/shift that they work. But at the time they're calling me it's all about patient care and getting done what needs to get done. I was a third shift tech for many years so I know what it's like to be having a problem in the middle of the night and needing someone to ask for help. Luckily no one abuses the courtesy of having me available 24/7 so it's never been an issue for me.12 points -
Reagent fridge holder
Reagent fridge holder
John C. Staley and 11 others reacted to tbostock for a post in a topic
12 pointsWe used some foam packing material and cut it into squares and they fit snugly in the channels of the rack. #boom12 points -
Barriers to understanding
Barriers to understanding
Maureen and 11 others reacted to Dr. Pepper for a post in a topic
12 pointsAll this just reinforces my opinion that one should never, never, ever get sick, because then you can get treated and all sorts of bad things can happen!12 points -
sending patient samples to a reference lab
sending patient samples to a reference lab
mmcfaddin and 11 others reacted to John C. Staley for a post in a topic
12 pointsI wish I had a dime for everytime I wanted to transfuse a patient just so I could get their antibody levels up to a point I could easily identify them!!! Never did but sure thought about it.12 points -
Anti-G anyone?
Anti-G anyone?
AuntiS and 11 others reacted to Malcolm Needs for a post in a topic
12 pointsHi Sara, The first clue that the antibody may be anti-G, or anti-C+G, rather than anti-C+D, is indeed that the titre of the anti-C is higher than that of the anti-D, but the fact that the anti-C titre is higher than that of the anti-D is only a clue. It could be that you actually have an anti-C+D where, coincidentally, the anti-C titre is higher than the anti-D. It is absolutely essential, therefore, that you can prove that no anti-D is present. One way of doing this is to divide the patient's plasma sample into two. The first sample is adsorbed using Ro red cells treated with a proteolytic enzyme, such as papain or ficin, which would adsorb out any anti-G and any anti-D present, but would leave any anti-C present. At the end of the adsorption process (about 4 cycles), this plasma is tested against r'r red cells by IAT. If there is a positive reaction, then the original plasma contained anti-C and, possibly, anti-G. If there is a negative reaction, then the original plasma contained, possibly, anti-G and anti-D, but not anti-C. The second sample is adsorbed using r'r red cells treated with a proteolytic enzyme, such as papain or ficin, which would adsorb out any anti-G and any anti-C present, but would leave any anti-D present. At the end of the adsorption process (about 4 cycles), this plasma is tested against Ro red cells by IAT. If there is a positive reaction, then the original plasma contained anti-D and, possibly, anti-G. If there is a negative reaction, then the original plasma contained, possibly, anti-G and anti-C, but not anti-D. So, if there are no reactions with the plasma adsorbed with Ro red cells when tested with r'r red cells, and no reactions with the plasma adsorbed with r'r red cells when tested with Ro red cells, then the original plasma contained only anti-G. If there is a reaction with the plasma adsorbed with Ro red cells when tested with r'r red cells, and also a reaction with the plasma adsorbed with r'r red cells when tested with Ro red cells, then the original plasma contained both anti-C and anti-D (and may also have contained an anti-G). In all cases, however, you would give cross-match compatible C Negative, D Negative blood (you would still have to perform a serological cross-match, because there are some EXTREMELY rare donors around who are C Negative, D negative, but G POSITIVE. As far as obstetric patients are concerned, both anti-C and anti-G usually cause far less severe haemolytic disease of the foetus and newborn (unless they have an unusually high titre), than does anti-D. However, it is important that the pregnant lady is offered prenatal and postnatal anti-D immunoglobulin prophylaxis, so that they do not get immunised against the D antigen. I hope that this rather long and complicated post helps in some way, but, if you need to know more, please do not hesitate to ask more questions.12 points -
Historical Record Check - How to prevent errors from misregistration?
Historical Record Check - How to prevent errors from misregistration?
KarenJ and 11 others reacted to John C. Staley for a post in a topic
12 pointsTime for a little philosophy. I have often described healthcare as an upside down pyramid with everything balanced on it's weakest part. Generally speaking, and I really intend no disrespect here but, our entire system is at the mercy of the lowest paid, least educated areas with the highest turn over rate. You will rarely encounter a career admissions clerk. Their training generally consists of "see one, do one, teach one". Granted this is based on my limited personal experience but it is what I and my wife have both seen in our careers in healthcare. As to a solution, I'm sorry to say that I don't have one that is very palitable in the current climate of financial restraint. (How is that for attempting to be PC!) I have found over the years when ever the opportunity to educate those folks responsible for obtaining patient information on why it is so critical, from a blood bank perspective, to get it right they were quite surprised and became much more diligent. Which brings me to another of my favorite axioms, "If they don't know why they can't or won't comply!" Ok, I'm done. Have a nice day.12 points -
+s in Ortho panel
+s in Ortho panel
traci89 and 10 others reacted to Malcolm Needs for a post in a topic
11 pointsThe +s stands for strongly expressed. The expression of the P1 antigen varies considerably from person to person, but the reaction strength with anti-P1 is an inherited trait (i.e. the strength of the expression on the red cell surface). "I apologize for this dumb question." BBnoob69, NO QUESTION IS A DUMB QUESTION, IF YOU DO NOT KNOW THE ANSWER. If you don't know the answer, the dumb thing is to not ask the question in the first place. NEVER be afraid to ask a question on here,11 points -
Incompatible Blood
Incompatible Blood
tesSBB and 10 others reacted to jayinsat for a post in a topic
11 pointsYou did everything that was required in this situation. The patient was a trauma and needed emergency transfusion. The risk of death outweighed the risk of a hemolytic transfusion reaction in that scenario, according to the treating physician. I once had a trauma surgeon tell me "I can treat a transfusion reaction but I can't treat death!" That put things in perspective for me. That is why thy sign the consent. Next step would be to report this to your risk management department so that follow-up can be made, including monitoring the patient for the s/s of DTR.11 points -
Does anyone knows what does “+s” mean?
Does anyone knows what does “+s” mean?
DLabGirl and 10 others reacted to Malcolm Needs for a post in a topic
11 pointsIt simply means that the P1 antigen is particularly strongly expressed on these red cell samples. Therefore, if you come across a weak anti-P1, it may apparently react with these particular red cell samples, whilst apparently not with, for example, the third red cell sample shown in your antigram. Although not identical to dosage, per se, it is fairly synonymous with dosage at a phenotypical level. The strength of the expression of the P1 antigen is an inherited trait.11 points -
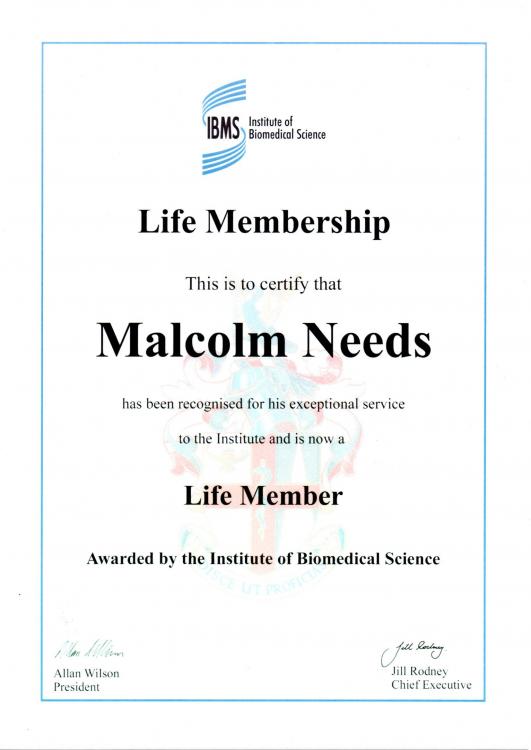
Life Membership of IBMS.
Life Membership of IBMS.
SbbPerson and 10 others reacted to Malcolm Needs for a post in a topic
11 pointsVery proud to have received this through the post earlier this week, to go with being elected to Fellowship of the British Blood Transfusion Society earlier this year.11 points -
Transfusing Blood in the OR
Transfusing Blood in the OR
Carol Salo and 10 others reacted to John C. Staley for a post in a topic
11 pointsThis is not a popular concept but at some point we have to accept there are things we can not control. Once the blood leaves the blood bank we are at the mercy of other humans and as long as the human factor is involved there will be human error be it unintentional or intentional. Attempting to complicate a process will only provide inventive humans the opportunity of coming up with creative work arounds to circumvent your best of intentions. At some point you just have to step back, do your job and hope for the best. I had a corporate transfusion QA director who could not accept that human error could not be completely eliminated with out eliminating human involvement in the process. Her directives became horribly complex solutions with multiple, redundant checks and balances only resulting in increasing problems. Bottom line, pick your battles and fight those you have a reasonable chance of winning. Make suggestions, offer insight, provide training opportunities but at the end of the day realize that you have to accept some things are simply beyond your control and even your influence. On that happy note I'll step off my soap box and stop my philosophical ramblings.11 points -
CORD BLOOD NOT MATCHING HEEL STICK TYPE
CORD BLOOD NOT MATCHING HEEL STICK TYPE
Eman and 10 others reacted to Malcolm Needs for a post in a topic
11 pointsIf you put a drop of blood on something like a filter paper, and then add a drop of 1M NaOH, if it is adult blood, after a couple of minutes it will turn a sort of yellow/brown colour, as the Hb is denatured by the alkaline, whereas, if it is blood derived from the baby (including cord blood), the red cells will stay red, as HbF is not denatured by the alkaline for much longer. It is rather like doing a Kleihauer, but by "bucket chemistry", as it is known!11 points -
YAY! THE LIGHTS ARE BACK!!
YAY! THE LIGHTS ARE BACK!!
Maureen and 10 others reacted to mollyredone for a post in a topic
11 pointsTHANKS FOR THE CHRISTMAS PRESENT! FRUSTRATION RELIEVER!11 points -
SIGNIFICANT ANTIBODIES FOR ELECTRONIC XM
SIGNIFICANT ANTIBODIES FOR ELECTRONIC XM
AMcCord and 10 others reacted to Malcolm Needs for a post in a topic
11 pointsSo, the easy questions first eh Mari?????!!!!!!!!!!!!! Personally, I think the IT guy gave you a poisoned chalice. The reason I say this is because we can all list antibodies that are not generally considered to be clinically significant, and then, all of a sudden, one comes along amongst these specificities that has not read the appropriate text books and goes ahead and causes a clinically significant reaction. Then what happens is that the person who said "anti-X" is not clinically significant, and this single example of anti-X turns out to be clinically significant, and you have to defend this in court. The real problem these days is that the technologies available to us are now much more sensitive than when I started (when cross-matches were recorded on a stone slab with a hammer and chisel) and many antibodies that were not clinically significant (because we just didn't detect them with the technologies available at the time) are now readily detectable - BUT, they are not necessarily detectable at strictly 37oC, as , for example, many examples of anti-M are now detected by "IAT", even though they do not really react (in real terms) at 37oC. The real problem comes when, for example, an anti-M genuinely DOES react at 37oC, and it is treated as clinically insignificant, electronic issue is used, and one or more of the units is M+ and the patient has a severe reaction - who answers in court? The worrying thing is that there have been papers published over the last few years quoting an anti-Leb as causing a transfusion reaction, and an anti-P1 causing a transfusion reaction (a certain Garratty G being a co-author on this one). I would say, therefore, that the best thing to do is to read through the relevant parts of The Blood Group Antigen FactsBook, Human Blood Groups and Mollison's Blood Transfusion in Clinical Medicine (latest editions in each case), and use their experience, rather than your own (no insult intended) as the courts would probably take the authors as "experts" should you come across any of these clinically significant "outliers". I wish you the very best of luck!11 points -
Positive DAT
Positive DAT
galvania and 10 others reacted to Malcolm Needs for a post in a topic
11 pointsIn my opinion, this very much depends upon the underlying pathology. For example, if the patient has an auto-immune haemolytic anaemia, the chances are very strong that the DAT will be positive before as well as after the transfusion, and that any eluate will be positive with all red cells tested (of normal type). The chances of detecting a new antibody specificity on the DAT positive red cells under these circumstances is disappearingly small. Therefore, if the sample is sent to a reference laboratory on a regular basis, your manager will be 1) showing a degree of ignorance that should be surprising, 2) will be upsetting the staff of the reference laboratory, as most have enough to do, without having to perform extra, unnecessary work, and 3) as you are in the UK, will be wasting the tax payer's money (and, as a UK tax payer, I feel very strongly about this). If, on the other hand, the positive DAT is new, then a reference laboratory would be delighted to help out. Of course, what your manager could do is to buy his/her own laboratory an elution kit, and train his/her staff to use it!!!!!!!!!!!!!!!! This may bring the cost of the kits to meaningful results ratio to the overall pathology manager, which could be of interest!11 points -
Nurses performing high complexity testing
Nurses performing high complexity testing
macarton and 10 others reacted to Moncada for a post in a topic
11 pointsAtt All: On behalf of pathologists and laboratory professionals, ASCP is urging the laboratory community and other interested individuals to Sign the Petition urging the Centers for Medicare & Medicaid Services (CMS) to reconsider its position that nursing is a biological science for purposes of performing laboratory testing. We ask that you forward this petition to all of your colleagues. http://cqrcengage.com/ascpath/app/sign-petition?0&engagementId=239813 Here is the link to sign this important petition!11 points -
Changing Venue
Changing Venue
AMcCord and 10 others reacted to David Saikin for a post in a topic
11 pointsJust wanted to comment that starting 6/27/2016 I will become the interim Blood Bank Manager for the Cottage Hospital system in Santa Barbara, California. Looking forward to the challenges and opportunities this will bring my way.11 points -
Transfusion Record
Transfusion Record
MaryPDX and 10 others reacted to Malcolm Needs for a post in a topic
11 pointsIf the information is required, then it is required. If the nurses can't be bothered to fill it in, go down the disciplinary route. If the information is NOT required, then ditch that bit of the form.11 points -
Cold antibody detection
Cold antibody detection
MinerJ and 10 others reacted to Malcolm Needs for a post in a topic
11 pointsWell, there are two reasons. The first, and main reason, is that we don't want to detect cold antibodies in the first place, because, unless they react at 30oC or higher, they are most unlikely to be clinically significant. Therefore, detecting them, and then having to investigate them for specificity is a complete waste of time and reagents - and staff time is the single most expensive thing in the laboratory. Secondly, it is highly unusual that you would only detect an IgM antibody by the presence of activated complement (not impossible, but highly unusual) and, therefore, the fact that EDTA chelates the Ca++, Mn++ and Mg++ ions required for the complement cascade to initiate, is irrelevant. The IgM molecules will still be present in the plasma, and are normally easily detectable. As I said above though, obviously, if we are trying to detect the biphasic anti-P that causes PCH, we would need complement present, and we would then use serum - BUT, very often in these cases, the patient's own complement is already exhausted, and so we would use the indirect two-stage DL test, where fresh complement from another source is added.11 points -
Congrats to Heather Vaught
Congrats to Heather Vaught
Sandy L and 10 others reacted to tbostock for a post in a topic
11 pointsJust read this month's AABB News and saw Heather Vaught's name, a member of PathLab Talk: Heather Vaught, MLS(ASCP)SBB, director of technical operations at Indiana Blood Center in Indianapolis, was recently recognized as one of the "Top Five" in the 40 under 40 list from the American Society of Clinical Pathology. Congrats from your PathLab Talk friends!11 points -
Questions about a potential A subgroup
Questions about a potential A subgroup
KatarinaN and 10 others reacted to Malcolm Needs for a post in a topic
11 pointsHi Amy, My first thought was, why did the overnight person give group A blood, rather than group AB? But, perhaps you do not carry group AB in your stock. Between 1 and 2% of the random White and Black population are A2B, and of those, only 25% produce an anti-A1. An anti-A1 that is clinically significant (reacts at 37oC) is disappearingly rare, so I wouldn't worry about it, but why switch to group O? The ABO antigens are not direct gene products, but are the result of the action of transferase enzymes that ARE direct gene products (give or take a bit of post-translational jiggery pokery!) and the A transferase and the B transferase compete with one another to put their own terminal sugar residues on to the Type 1 and Type 2 backbones, and it is not unusual for the A antigen to be weaker than the B (so that an A1 reacts more strongly with anti-A than does an A1B, and an A2 reacts more strongly with anti-A than does an A2B). This patient is also an elderly oncology patient, and both age and his condition can affect the expression of ABO antigens. I would switch back to group A for transfusion if I were you (or, better still, AB).11 points -
Bit of a rant....
Bit of a rant....
mewilde1 and 10 others reacted to Dr. Pepper for a post in a topic
11 pointsAuntie and others, we share your pain. If I may add to the list of pet peeves: 1. Starting weekly temperature discs on fridge/freezers on the wrong day and/or time. Then 5 days in a row 5 different techs document that the scribe is OK. 2. Not recording medical record numbers and dates on panel scoresheets. Record keeping in general. 3. Not printing copies of panel scoresheets on both sides so you get the extended antigen typings on the the back. Not changing the scoresheets when you open a new panel lot. 4. Filing QC records etc. with bloodstains (hopefully reagent but you never know) all over them. 5. First cousin to the above: finding blood all over the counter, centrifuges, agglutination viewer, outside of the biohazard bin, drawers or cabinets, making you wonder if a worker had been shot or merely had sneezed violently during a torrential nosebleed. 6. Discarding packing lists from the blood center so I have to get copies to check the bimonthly bill. Happens pretty much each cycle. 7. Finding obviously broken thermometers, pipettors etc. in place. Whoever broke them knew they had done so but decided to keep it secret.. 8. Not telling you when the last kit, vial, package, bulb or box was opened so you might have a ghost of a chance to order more before you run out. 9. I put out a half dozen pens and markers a week. Where do they go? Even if we supply the whole lab we should have reached the saturation point decades ago. 10. A tech asked me if it was OK in a pinch to just use one drop of plasma/serum per tube for an antibody screen; another tech had told him that was fine if you didn't have much sample. This was right before last year's competency eval, so I included that as a question. 5 people said it was OK. So we had a little inservice on the value of following the manufacturer's directions, our own P&P, and the need to validate any variations in protocols etc before you do so. I heard a great line a few years ago that went something like "Ignorance ain't what you don't know; it's knowing too many things that ain't so!" Thank you, I feel better.11 points -
Storing Saline Cubes
Storing Saline Cubes
jshepherd and 9 others reacted to albaugh for a post in a topic
10 pointsI think you should invite members of that committee to remove a bag from its cube, try to label it sufficiently (substance, lot #, expiration, etc.), attach that label in such a way that it will stay attached when the bag 'collapses' as it's emptied, hoist the bag up to the level of a cell washer without the aid of the box (especially this part), and suggest ways to keep the collapsed bag at an angle that will ensure all the contents are used. I'm willing to bet they'll come around.10 points -
CAP survey data entry
10 pointsFound early mornings and evenings are best. A martini in hand doesn't hurt either.10 points
-
Bg antibodies
Bg antibodies
SbbPerson and 9 others reacted to Malcolm Needs for a post in a topic
10 pointsBg antibodies are antibodies directed against HLA Class I antigens. These antigens are expressed quite strongly on virtually all nucleated cells, but are poorly expressed on red cells. This is purely down to the number of antigens sites on the various cells. For example, a T lymphocyte will express some 100, 000 such antigens on their surface, whereas a red cell will only express from 40 to 500 such antigens. It was originally thought that Bg antigens on red cells were adsorbed onto the red cell surface from the plasma, but it now seems that these antigens may be intrinsic, having been formed during the time when the erythrocyte precursors actually had a nucleus, but, that notwithstanding, they can easy be removed from the red cell by chloroquine treatment. Bga is analogous with HLA-B7, Bgb is analogous with HLA-B17 and Bgc with HLA-A28, but there may be cross-reactivity with other HLA antigens. Bg antibodies are very common in pregnancy, having been stimulated by the foetal HLA antigens, but have never been implicated in clinically significant HDFN, so neither you, nor the expectant mother need to worry (they are "nuisance" antibodies). For more information, try Geoff Daniels, Human Blood Groups, third edition, 2013, Blackwell Publishing Ltd. Chapter 32 (pages 512 - 514) - so there is not a lot to read!10 points -
Anti-Cartwright b antibody
Anti-Cartwright b antibody
CMCDCHI and 9 others reacted to Malcolm Needs for a post in a topic
10 pointsHi Kelli, Reid ME, Lomas-Francis C, Olsson ML, The Blood Group ANtigen FactsBook, 3rd edition, 2012, Academic Press, states that anti-Ytb causes neither haemolytic transfusion reactions, nor HDFN. Daniels G, Human Blood Groups, 3rd edition, 2013, Wiley-Blackwell states more or less the same (but does state that monocyte monolayer assays do predict the possibility that some examples of anti-Ytb could cause premature red cell destruction, but not a clinically significant haemolytic transfusion reaction). It should be noted that the MMA is no longer performed, to any great extent, in the UK, as it has been found to be unreliable. If you put "Daniels Clinical Significance of Red Cell Antibodies" into your search engine, one of the things that springs up is an NHSBT Specification Document, written by Geoff, entitled "SPN214, Clinical SIgnificance of Blood Group Alloantibodies.", in which Geoff says that it is safe to give cross-match compatible blood to a patient with anti-Ytb, rather than get Yt(b-) blood. It is a useful document to download. Carolyn Giles, who discovered anti-Ytb, and with whom I had the huge honour to work with when I was younger (and more junior), never regarded the antibody as clinically significant. I would suggest, therefore, that the raised LDH and lowered haptoglobins is either a coincidence, or evidence of a subclinical haemolytic transfusion reaction (i.e. the red cells may not be lasting as long in the circulation as may be expected, but their destruction is slow and is not causing a clinically significant haemolytic transfusion reaction). I hope that helps.10 points -
Roseburg college shooting
Roseburg college shooting
Lbiggs and 9 others reacted to mollyredone for a post in a topic
10 pointsThanks everyone! We have had an incredible outpouring of support. They are calling one of the injured victims a hero for rushing the gunman and saving people-he was shot 5 times! After the first three shots, he fell and told the gunman it was his son's birthday and was shot 2 more times. Roseburg is also the home of one of the Americans who stopped the terrorist on the train in France. He works at Costco here. People are amazing!10 points -
The 30 minute rule
The 30 minute rule
Sandy L and 9 others reacted to Dr. Pepper for a post in a topic
10 pointsThere are always things that make you scratch your head a bit, that you dare not go above 6o for a second during storage, but that 10o is fine during shipping. Or that you cannot send RhIG through the pneumatic tube because it might be subjected to undue turbulance, but the shipper can kick the hell out of it and throw it in the back of a truck with bad shocks to jiggle along a bumpy road on its way to you.10 points -
Does the strength of a reaction correlate with the severity of a fetomaternal hemorrhage?
Does the strength of a reaction correlate with the severity of a fetomaternal hemorrhage?
aafrin and 9 others reacted to Malcolm Needs for a post in a topic
10 pointsI would agree that there is no correlation between the strength of the DAT and the severity of the HDFN (ABO HDFN quite often has a negative DAT), but I would thoroughly disagree with the comment that a weak DAT means that there was a smaller foetal bleed. There is very little correlation between the amount of the foetal bleed and the strength of the maternal antibody. There is much more correlation between the immunogenisity of the foetal antigen and the strength of the maternal antibody.10 points -
How to determine subgroups of ABO blood groups
How to determine subgroups of ABO blood groups
watsbj and 9 others reacted to Malcolm Needs for a post in a topic
10 pointsI am somewhat surprised that you "often" see patients with these subtypes as, working in a very large Reference Laboratory, we see no more than about 2 or 3 a year. That having been said, with the advent of avid monoclonal grouping reagents, it is now almost impossible to assign a specific subgroup to an individual, without the use of molecular techniques. The old way of assigning such subgroups is somewhat defunct, as the reactions we get with these modern monoclonal antibodies are so much stronger than those seen with human-derived polyclonal reagents (and even then, the "strength of the reaction" tended to vary from one laboratory to another, and from one person in a laboratory to another, as the reading was totally subjective). Personally, I would not now attempt to assign a specific subgroup. As long as the patient is, say, group A, it really doesn't matter if they are A1, A2, A3, Ax or Am. They can still be transfused with group A1 blood, unless they have an anti-A1 in their plasma that reacts strictly at 37oC, and such an antibody is extremely rare. If there is any doubt, they can be given group O blood. From the donation point-of-view, again it doesn't matter if the donor has a subgroup of, for example, group A; they are still group A, and, as a consequence, their blood should be labelled as such, so that it does not go to a patient who is group O or group B.10 points