jayinsat
Members
-
Joined
-
Last visited
-
Country
United States
Everything posted by jayinsat
-
Ortho Vision Antigen Testing
@DARREN, can you order partial sleeves from Ortho? Will they sell them in smaller packages? Another thought is, if you are part of a system, perhaps you can get your supply of cards from your sister facilities that use more volume. That would alleviate the wastage. Just a few thoughts.
-
Use of plastic tubes for tube testing
@Sonya Martinez, I also would like to know who it is telling you this. My guess is it is some infection control nurse during an inspection that has no idea about immunology, just following a checklist. I experienced that years ago and simply pointed them to similar information that @Malcolm Needs stated. I have always been taught that plastic tubes were not acceptable in blood bank for that reason.
-
Patient with WAA unable to determine ABO & Rh type
Hi Malcolm, What terminology is recommended in these situations? We have always used "least incompatible" in the states. I think, probably, the majority of our databases have that option listed besides "compatible" and "incompatible." What terminology should replace "least incompatible?"
-
Positive crossmatch
My initial thought is check for ABO compatibility, which is what exlimey is suggesting. How was the Jka antigen testing performed? Were controls run and did they work? Also, perform a DAT on the units. If they are DAT positive, your crossmatches are invalid. I doubt that would be the issue though. 4 donors all having positive DAT's? If you had a clear anti-Jka identified, and all other antigen groups ruled out homozygously, there is no reason the units should be XM incompatible if they are ABO matched.
-
Positive Culture on Platelet Unit
I would treat this like any other lookback or non conforming product notification from my supplier. I would generate a risk management occurrence report and submit it to our medical director. Our medical director and the patient physician would figure this all out.
-
Why irradiate liquid plasma when RBCs for trauma patients aren't irradiated?
To add to the this thought, the low titer O whole blood currently being used in many trauma situations is not leuckoreduced or irradiated. Seems to me that it is time to rethink the need to irradiate in trauma situations.
-
Temp of units while receiving to inventory
Is there a new checklist item that is asking about this? Otherwise, I see no need to record this. We do not record the temp when it is out for antigen typing or any other tests. Why do it here?
-
Positive Baby DAT and Fetal Screen
Danielle, I love the lights. When i'm feeling stressed, I come here and break em. If you haven't noticed, move over them with your mouse and they break with the most refreshing sound of glass breakage. I hope you all don't think less of me now...
-
Positive Baby DAT and Fetal Screen
I would consider this a non-issue as you would need to quantify any positives with a KB stain or flow cytometry anyway.
-
RHIG Dispense from Pharmacy
We moved rhogam to pharmacy more than 10 years ago for all 7 of our hospitals in our system. It has been great! It poses no more issues than any other transfusion or lab related process that is under other-than-lab control (POC, transfusion administration, etc). We get a report printed from pharmacy (autogenerated) every morning that inform us when patients received rhogam, fludara, or IVIG. We print a report daily in blood bank that shows all rhogam candidates (females of child bearing age that typed rh negative). The patients on that list are evaluated to see if they were rhogam candidates and if the workup has been ordered (if necessary) or dispensed. Our L&D and ED have very little problem with the process. There is the ocassional missed dose or inappropriate dose in ED but that is relatively rare and has been the same as before moving it to pharmacy. My experience is that it is better in pharmacy than blood bank. Your mileage may vary.
-
Blood on Helicopter
I work in a San Antonio hospital and what was reported at AABB was the expectation. It is NOT the reality. First, all units supplied to the ambulances and helicopters come from our regional donor center. No hospital transfusion service provides the units nor are we responsible for the disposition of the same. All of this is monitored and tracked by the regional donor center and the EMS. What is supposed to happen is, when a patient has been transfused en route, the completed unit and EMS's transfusion form is supposed to be sent to the blood bank upon arrival. This almost never happens. The only way we know in the blood bank is when we get mixed field reactions on our blood type or by reading physician notes on the chart. I read the physician note of every emergency release. That is how I normally find them. The physician will dictate that the patient received blood in the ambulance. It takes days for me to track down the paperwork and the empty bag is long gone by then. We NEVER crossmatch them because we never receive them. All that said to say, your helicopter company needs to contract with whomever your blood supplier is to stock the units. That should not come from the transfusion services department of the local hospital. You might serve as a pass-through site, meaning the donor center uses you as a pick-up point but the units are never part of your inventory.
-
Pick Up Slips to request blood from Transfusion Services
O.R. has forever been, and forever will be the weakest link in transfusion services. As was previously stated, there are a lot of moving parts and many of those vital parts have no computer access since they are contracted workers. For instance, the perfusionists and anesthesiologist have no computer access since they are only here for the case. All orders are verbal orders. They are the ones starting and ending the transfusions. There is no computer in the suite, everything is done at the desk by the circulating nurse. We have fought for decades to change that process but have had no success. Everything is manual in O.R.
-
New Site for Blood Transfusion History.
Awesome site Malcolm. I was just reading the 1668 letter Acton, G. (1668) Physical reflections upon a letter written by J. Denis, professor of philosophy and mathematicks, to Monsieur de Montmor, counsellor to the French King, and Master of Requests concerning a new way of curing sundry diseases by transfusion of blood. London. Early English Books Online Text Creation Partnership. https://quod.lib.umich.edu/e/eebo/A26307.0001.001?rgn=main;view=fulltext. Wow! How far transfusion medicine has come. I am glad I was born in the 20th century instead of the 17th century.
-
Antibody Screen Tube method
I agree with Malcolm. I haven't worked in a blood bank that routinely performs IS, or 37C readings in a long time. None of the instrument manufacturers antibody screens include them either. Your supervisor is helping you. You should thank her for saving you unnecessary work.
-
Infant transfusion units
We do about 6 NICU transfusions/year. We routinely keep a fresh, CMV=, IRRADIATED unit on hand which is replaced every week. That unit is for emergency transfusion only in the NICU. If the situation is not critical, we order a fresh unit for the baby with satellite bags attached. It takes our supplier about 90 minutes to get that unit to us. The majority of our babies can wait. If it is an emergency, then we give the best product we have. The neonatologist says "we can treat hyperkalemia but we can't treat death."
-
Anti-CD38 therapy discontinued
We do not unless the patient has Anti-K. Darzalex is just a transient interfering substance. If there is no DTT neutralization required and no antibody detected, it is not necessary. Plus, I don't see how I can charge for the antigen typing in that scenario. I think that risks fraudulent billing.
-
Documents - How long do we need to save ?
I agree with David. Pick-up slips information and blood orders are all electronic and maintained in the LIS or the donor centers order website. CAP requires 10 years for blood and inventory inspection records, which includes shipping documents, since they usually contain a message about shipping, storage, and inspection.
-
patient history cards
BB.rick, I would have no problem retiring the card system in your case provided that you are regularly (daily) downloading a copy of the records to a secure, accessible file for downtime. Also, make sure all staff know how to access that data for prolonged downtime. There is no reason to have a card system with Meditech. BTW, my previous position was in a place where the manager refused to stop using the card system. It was mainly because they were not familiar with how to access the information during Meditech downtime. Even when shown how, they still refused. It is still in use today at that site. Some battles you can't win.
-
transfusion competency of on-call staff
In the USA, there is an extreme shortage of techs that are blood bank competent. The ones who are are working regular overtime to fill in the shifts to provide 24/7 coverage. They are normally working at least two jobs. The field is facing a crisis as these techs who are qualified are now retiring. We just lost two of our best this year and are struggling to keep the younger, promising techs in the field. I'm afraid you won't really have a choice soon. You will have to take what you can get tech-wise and train them as best you can.
-
Thawed Plasma ISBT Code
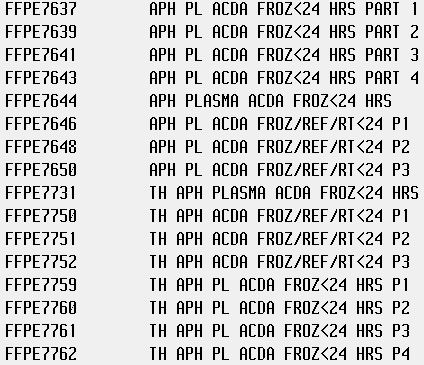
You cannot use E2121 for all of them. Each of those frozen products have a corresponding thawed 24hour and a thawed 5 day plasma code of their own. You have to use those. We go straight from frozen to 5 day thawed so we only use those two. Here is a screen shot of our database.
-
CAP staff competencies
CAP competency requirement is labor intensive, regardless of how you document. I have been trying to put more on their competency assessment tool they offer. Setting that up alone is labor intensive. It is the number 1 cited issue of most labs in America. It is not that we are not competent, of course. We have a hard time showing it the way CAP wants it. It really requires a full time QA position just to keep up with the competencies of all the staff in every department.
- Barrier method
-
Thermometers for taking temp of returned blood products
We just switched to the MaxQ MTP coolers and love them! My validations showed it held temps for 24 hours, even when opening the lid every 15 minutes for the first 2 hours and hourly after that. Plus, we filled the cooler with warm FFP (4 units @37C) and cold RBC (4 units @4C). The cooler cooled down the FFP units to 6C within 3 hours. The RBC'S never went above 5C.
-
Thermometers for taking temp of returned blood products
We use 1-6 for coolers, however, the BT-10 only shows breach above 10 so, there's that. We place a NIST certified thermometer in the cooler to show that it is 6 or below upon return. We do not scan these units with the temp gun. It's 1-10 for anything returned not in a cooler.
-
Thermometers for taking temp of returned blood products
We use one from Fisher. It is certified and we replace it every 2 years when the certificate expires. I am curious, for those who have the 15 minute limit, did you validate that in all scenarios in your hospital?