-
-
-
-
-
Preadmit Specimens
We have an Extended T/S form used in Pretesting. The nurse will ask the patient if they have been transfused or pregnant in the last 3 month. Nurse signs the form and answers Yes or No. The form along with T/S specimen is sent to BB. We do the testing that day and indicate on the form if the patient has a BB history. If not, we will need an ABO Recheck specimen collected the morning of surgery. We put a round sticker on top of the specimen so we don't discard accidently. We place a comment in the computer that the patient has an Extended T/S for our info on the day of surgery. Two days before scheduled surgery, we fax the forms to Surgery Holding. Holding wants these early so they can make up the charts the afternoon before surgery when it is not so hectic. Day of surgery-Nurse asks the transfusion and pregnancy questions again, signs the form and collects the ABO Recheck specimen if needed and faxes the signed form to us. We also send a list to Surgery Holding of all the patients we know needs an ABO Recheck collected while IV is being placed so we can be sure they get the message before the patient is rolled away The BB will find the preadmit specimen in storage & test the ABO Recheck, if needed. We have a special BB order we place in the computer to answer some of the questions about the pretesting. The XM now gets 3 days and the preadmit specimen has the sticker pulled off the top and is placed in storage with all of today's specimens. In this process, we remove the comment from the computer. We will extend up to a month, so 30/31 days so we don't have to count on our fingers. LOL. If the patient comes in for surgery past the 30/31 days, we request a new order and specimen. If the patient turns out to have an antibody, we will ID and write the info on the form and hang the form up for all BB to see. We will scan for Ag- neg units prior to surgery. We write a BIG note on the form that we want a FULL pink top collected on the day of surgery and redo the T/S and crossmatch the units. We don't redo the AB panel as long as the screen appears as expected, plus the patient hasn't been transfused. It takes 3 departments completing their tasks but it works like a charm after the initial learning curve. We do not use BB armbands so I'm not sure how that would work. I don't see people wearing an armband for a month or requiring a patient to bring the armband with them on the day of surgery. Maybe some of this info can help you.
-
Critical values
Things I have listed in my procedure: 1. If we have discovered an antibody on a patient who is about to go to surgery, we call the nurse in charge of the patient in Surgery Holding to let the physician know blood may not be available. The doc needs to know before the patient goes under the knife. Sometimes they delay the surgery and sometimes they proceed with caution. (This issue can be avoided with a pretesting process that not all physicians use) 2. If we have a serious transfusion reaction due to ABO incompatibility, we would contact the patient physician and our pathologist immediately. 3. We can't ID the antibody and the physician has requested RBC transfusion. Depending on the condition of the patient, they may still proceed with incompatible or least incompatible blood and sign a Medical Release or will probably wait until we can ID. It is up to the physician to make the call based on the patient. 4. When we had babies, we considered a positive DAT as a critical result from the BB side and would call L/D.
-
-
- Blood unit patient label
-
-
-
Blood unit patient label
We use a paper tag with a pre-attached sticky label. The tag has all kinds of info printed on it for the nurses edification, such as transfusion rxn info, only use saline, etc. The computer prints all the patient/donor info on the tag and also on the sticky label which we place on the unit at issue. The tag is primarily used at the bedside for the required checks but the unit itself is scanned into the computer and completed in the computer. If the computer is down or goes down, the nurse will revert back to the paper tag to complete the transfusion. The label stays on the unit throughout the transfusion. That has been beaten into their heads over the years. The tags are a specialty type print and are expensive but it is what it is. It took months of committee meetings to approve the tag we have now and every nurse had an opinion about what should be on the tag.
-
-
-
-
-
CAP ALL COMMON CHECKLIST COM.04250
I'm annoyed! Yes, there are differences in results between automation, GEL and tube testing. Automation is the most sensitive and tube testing is the least sensitive (but the BB gold standard method), with GEL in-between. I wrote that bit of information in my procedure so an inspector would know I am aware of the possible differences. We are doing this exercise to make sure the methods compare, if the specimen is positive in automation, it should also be positive in GEL and tube testing and should appear to be the same antibody on the antigrams. If I am doing an antibody screen and an AB ID, I am using the same METHOD whether I am testing using 3 screening cells or a panel of 10 or more cells. Yes, we have the rare antibody screen that gives wonky results in automation and and is stronger in GEL. That tells me we need to do the ID in GEL so we can actually get an answer we trust. Different antibodies work differently in different methods but the screen and AB ID should be the same within the same method. Our screening cell method in tube is the exact same method as our panel tube testing. If I am doing the comparability testing, I am using a strong antibody that has a 3-4+ result so I can be assured I will get similar results across all 3 methods. I'm not going to use a weak or wonky antibody that would give shady results an inspector could question when they view my forms at an inspection. This is Method Comparability, not Test Result Comparability. Does CAP have to have a quota of standard changes they have to meet? I'm on a soap box and I am sorry to rant but this seems unnecessary and extra work for the same AB screen results across the different methods.
-
Plasma Freezer Down: Better Process for Temp Storage of Frozen Products
This is awesome! As many times as our freezer has gone done over the years, we never thought of putting dry ice in the freezer. Your dad is awesome!!!
-
 DebbieL reacted to a post in a topic:
Plasma Freezer Down: Better Process for Temp Storage of Frozen Products
DebbieL reacted to a post in a topic:
Plasma Freezer Down: Better Process for Temp Storage of Frozen Products
-
CAP ALL COMMON CHECKLIST COM.04250
I get so annoyed when CAP "experts" give different answers to different people. It seems to me they also bring in their own personal opinion on things, like some inspectors we have to deal with. She stated she "suggests" doing ID on all methods I would have to argue they we are testing the "method." If you get a positive AB screen using automation, do you also get a comparable positive AB screen using GEL and tube? Does the antigram for the same antibody across the 3 methods appear to be the same antibody. It shouldn't look like an anti-E on automation, a anti-K in Gel and an M in tube. They are not going to match in strength because the different methods vary in sensitivity. I would include the antigrams of each method to show it appears to be the same antibody across all methods. A set of screening cells is just a mini AB panel. If you feel like you must do an antibody panel using each method, I would just do an extra cell or two on each method and say it is not a set of screening cells but a mini selected panel. If we find a patient with a good, strong, clear antibody it is sometimes hard to come up with lots of extra plasma to do unnecessary testing. (My opinion only) Gr-r-r-r-r!
-
Repeat of donor Antigen typing
We do not perform repeat antigen typing on units sent from the reference lab. If it says historical antigen type, we are OK with that. We enter the extra Ag typing into the computer when we receive the unit. We do not waste the time and antisera to retype units the techs type here at our BB. If I did that then why not go back and repeat everything else they did. The units would be AHG XM and should catch it if the antigen is showing up. If a tech did mislabel an Ag, they would be written up when it was found for causing patient harm. We once had a sickle cell frequent flier with an anti-E. Her antibody couldn't be detected after several years. Then she came in a few weeks later with a roaring 4+ ant-E. My first thought was we has mistyped a unit we had given her. After investigating, it seems she went to a wedding out of state and while she was there, she popped into a hospital to get juiced up. She neglected to tell them she had an antibody, even though we give out antibody cards. They didn't see the anti-E so just transfused her. That is the closest we have ever come to thinking we mistyped someone. I agree with Exlimey about repeating the ABO/Rh. I have worked for over 40 years and not once have I ever had a mistyped unit or even heard about a mistyped unit. I am guessing blood centers probably have multiple people type each unit to prevent labeling with the wrong type. It has always seemed like a waste of time to me. But it is a rule and we follow rules.
-
Facility location on SOPs
My previous boss always said they had to come up with new rules to justify their jobs. When they can't find the "low hanging fruit" because we all try hard to do the right things and follow the rules, they start digging deeper and come up with stupid stuff. As long as they keep coming up with new rules, they keep their jobs.
-
Facility location on SOPs
I had to look it up. I had never heard the word before but very relevant to the topic
-
Computer crossmatch validation plan
Keep a copy of the initial validation handy for CAP inspections. I was asked by an inspector to see it years after we had gone live. I had to dig through previous computer files from my previous boss to find it. It was my first inspection as a lead and made me so nervous. I think she was just messing with me to make me more of a basket case than I already was. Also anytime you have a major computer upgrade, you need to test all the computer elements again to prove the rules still work as expected. It doesn't take too long after you have the initial work down.
-
Storing Saline Cubes
We got the same song and dance from our infection department some years ago. Our manager told them the instruments would not work correctly if the saline/reagents were not in the manufacturer's container, the interior plastic bag would droop and possibly break without the cardboard support to contain it. The solution/compromise was to make a notebook of "acceptable" cardboard containers, e.g. saline/reagent cubes. If an inspector questioned, we would show them the book with pictures of what had to be in cardboard to maintain lot numbers or integrity of the reagent. I agree, the rule is to reduce incoming exterior dirt and insect infestation for patient areas but the lab is not a patient care area. Some committees make a mountain out of a molehill and go too far.
-
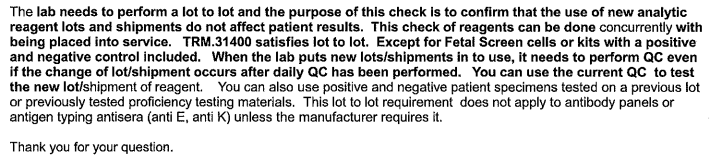
QC of reagents on receipt
There was a FAQ on the CAP site a few years ago that basically said BB did not have to do lot to lot testing, that our regular QC was sufficient. I know the exception was fetal kits or other kits that had positive and negative controls as part of the kit. I was concerned about this standard regarding our regular reagents after it was revised so I wrote to CAP so I could get an understanding if things had changed so we did have to start doing lot to lot. This was my answer for my question about COM.30450 The way I read this we do not have to do lot to lot except for something like a fetal kit. You can perform QC on the day of use. Part of our QC is to check the shipment upon arrival, is the appearance normal, did it arrive at the proper temp, was the shipping container damaged, etc. I like having an answer in writing with the CAP logo if an inspector seems like they are going to site me. I can whip the email out and show them. Might help, also might make them mad.
-
Antibody Screen Tube method
Thanks Malcolm! I looked closely at my screening cell package insert and was surprised that it no longer says to perform immediate spin. It says to perform a spin at 37C but if potentiators are used to follow their instructions. We actually use PEG instead of LISS and PEG is not supposed to be spun after incubation. I have looked at those inserts for years and never REALLY saw this wording and have no idea when these instructions changed. I knew we didn't really care about RT antibodies anymore but I thought the immediate spin was required. We have so many rules in BB and we just follow them without question. I feel like I am in an alternate universe right now.
-
Antibody Screen Tube method
This is news to me. Is there a reference to remove the IS and 37 reading. Is it only with a particular enhancement media? We currently use LISS. I would love to get rid of unnecessary steps.