Posts posted by Dansket
-
-
We are controlled, to a greater or lesser extent, by regulators as to what we can/cannot do. Talking with donor center personnel over the years, they have no 'wiggle-room' when it comes to compliance with FDA regulations. Transfusion Services inspections that are conducted by FDA surrogates are not nearly as stringent. Transfusion Services have the option to select a regulator (AABB, CAP, JCAHO, HFAP), Donor Centers have no choice.
-
17 hours ago, rravkin@aol.com said:
I was going to ask if distance traveled had anything to do with this distinction, transported or stored. But it is actually the container that is being transported and the blood is stored within this container. If the container is sealed such that the stored blood is not in any contact with the elements then the stored blood would be good until it's expiration provided the temp is maintained in this container. I think that the container's ability to maintain the appropriate temper for a given time and the time it takes to travel a given distance is probably where the question of transport and storage originates. But the temperature maintenance is a container issue and not the units of blood "stored within."
If a pregnant woman travels a given distance can we think that the fetus she is carrying is transported or stored?
The FDA's decision may have to do more with the level of control. Donor Centers are inspected directly by the FDA, whereas surrogates (AABB, CAP, etc.) inspect hospital transfusion services. As John C. Staley stated "This started being a hot topic 10-15 years ago." While Transfusion Services continue to challenge the FDA interpretations, Donor Centers don't!
-
Our SOP requires that newborns, who test negative with anti-D by immediate-spin test, must be tested for Weak D using anti-D antiserum formulated for Weak D testing. If the Weak D Control is agglutinated, we report Rh type of the newborn as "Indeterminate" and "RhIG indicated" for the mother if the mother is Rh negative.
-
-
Edited by Dansket
Added more questionsWhen user enters Type and Screen results into computer, are intermediate results entered (anti-A, anti-B, etc) or only the interpretations, e.g. APOS, BNEG etc.? Are results of Antibody screen for Cell1 and Cell2 entered or just interpretation, e.g. Positive or Negative?
-
We print an individual Results report for each specimen which is identified by a barcoded sample ID label affixed by the operator. The operator then scans the sample ID from the Results report into Meditech enters and files the results. The printed report is then filed in the Supervisor's Review basket.
As Supervisor, I repeat the process for each individual report and verify results on report match results entered in Meditech. I sign and date the report and file the report in a binder. This binder is made available for inspectors to indicate this Quality Review process.
-
An order for a second venipuncture is automatically reflexed by Meditech based on testing done on the initial blood sample collected for Type and Screen. Our phlebotomists have no role in determining whether or not a second blood sample is required.
If there is no ABO on file and testing of the initial blood sample with anti-A,B yields a positive test result (patient is not group O), Meditech automatically creates a new order for an ABO verification test that requires collection of a second blood sample. This results in printing of specimen collection labels on the Phlebotomy Label Printer.
Transfusion Services does not accept unsolicited blood samples collected for the ABO verification testing.
-
-
To prevent Meditech from qualifying a patient for EXM when mixed-field agglutination is detected, then detection of a mixed-field result must be entered into Meditech in some manner. In this way, Meditech can react to that test result using rules, reflexing tests, calculations and interpretations.
Currently, if mixed-field agglutination is detected in the Anti-A, Anti-B, Anti-A,B and/or Anti-D test, how is that mixed-field test result entered into Meditech?
What is your current policy for documenting selection of blood for transfusion in Meditech when mixed-field agglutination is detected in ABO/Rh grouping tests? For example, do you automatically select group O when mixed-field is detected in ABO grouping? Rh negative when mixed-field is detected in Rh grouping?
How is your Crossmatch test configured?
Do you use a Meditech Blood Issue routine in real-time when releasing blood to Nursing, et al?
-
-
-
-
-
3 hours ago, SMILLER said:
When we have this situation, we use a thermometer and set it next to one of the ice packs (as opposed to in between units). If the thermometer is off when the cooler is returned, we would check the unit with a digital thermometer before discarding it.
Scott
What temperature of the ice packs do you consider unaccepatable? What temperature of the unit do you consider unacceptable?
In the United States, holding Thawed FFP in a cooler is considered storage by the FDA. So whatever is the acceptable storage temperature of Thawed FFP would apply.
-
3 hours ago, BldBnker said:
I just have a hard time transfusing red cells that yield a 1-2+ positive reaction at immediate spin (can't call that compatible :o) ). ...
Let me spin this differently. I'm unlikely to detect an anti-A1 or any other weakly reactive (1-2+) IgM antibody in routine room-temperature gel testing. Secondly, I have eliminated the immediate-spin crossmatch in favor of an electronic crossmatch to detect ABO incompatibility between donor and recipient. Lastly, by adopting the electronic crossmatch, I have accepted that any reactivity (limited to room-temperature) between donor and recipient (not demonstrated to be due to anti-A and/or anti-B) is rendered clinically irrelevant!
-
On 6/18/2017 at 2:52 AM, Malcolm Needs said:
In addition, surely your computer programme should be written so that it helps you, rather than hinders you? It seems to me that, if the human being knows that group A blood, whether it be A1, A2 or any other subgroup of A, will be efficacious for the patient, the computer programme should not prevent the human being from giving that blood, and that the computer programme needs to be rewritten as a matter of urgency. This is particularly important to prevent the wastage of finite group O red cells, but more particularly, if the in vitro findings of Zaffuto et al are found to extend to the in vivo situation (or even if there is the slightest suggestion that they so do).
In Meditech, user can designate whether an antibody is/is not clinically significant and can also designate corresponding antigen-negatives. In the case of anti-A1, you could create two 'anti-A1' entries in the 'antibody file'. One would be designated "clinically-significant' and that A2 cells were 'antigen-negative'. The second entry in the antibody file would not be designated 'clinically-significant' and the 'antigen-negative' field left blank. For patients with an anti-A1 that reacts as 37C, computer would require A2 red cells for crossmatch. Patients with anti-A1 that does not react at 37C would not require A2 cells.
-
2 hours ago, R1R2 said:
Would it be acceptable to issue in the LIS and then tag the unit? Would that be breaking any regulatory requirement?
See my download in the library "Blood Issue Cause and Effect". The process starts with a tagged (form attached immediately after crossmatch) blood component removed from storage.
-
-
2 hours ago, Tabbie said:
Is there a standard way of performing an auto control ? I have seen an auto with rr panel cells. If someone could explain
Thanks
An autocontrol is an indirect antiglobulin test that includes both patient serum/plasma and patient rbc incubated together at 37C and subsequently tested with antihuman globulin reagent. Methodology includes the standard tube test, Gel test, PEG test etc.
-
I don't trust Nursing. They may have put the unit into storage on the Nursing station or mishandled the unit in attempts to warm it up or cool it down. I draw the line at 30 minutes, no exceptions. I don't get into "what if 31 minutes?, what if 32 minutes?, what if 33 minutes"?
According to your process, would you reissue blood returned unused and within temperature regardless of time out of storage? Are there no exceptions for time out of storage?
-
Edited by Dansket
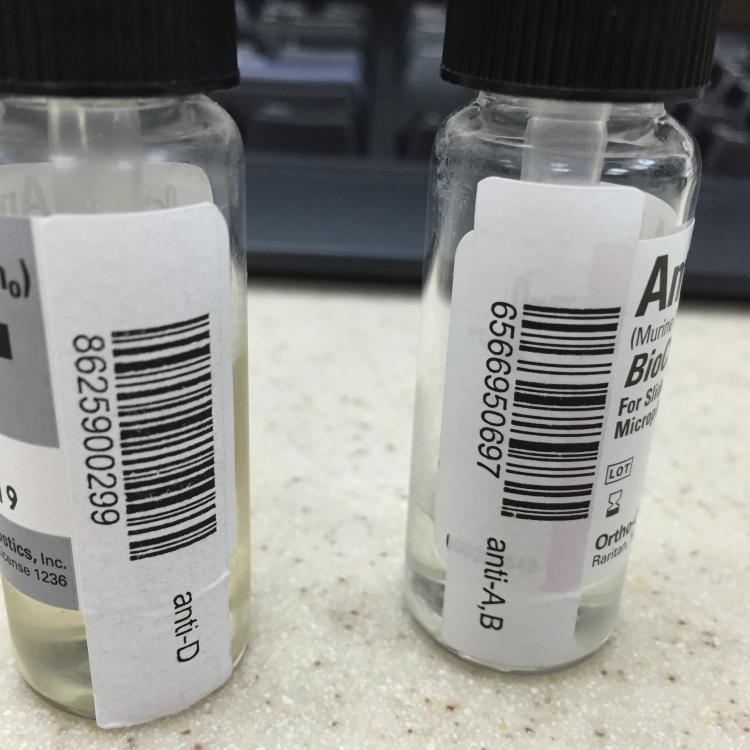
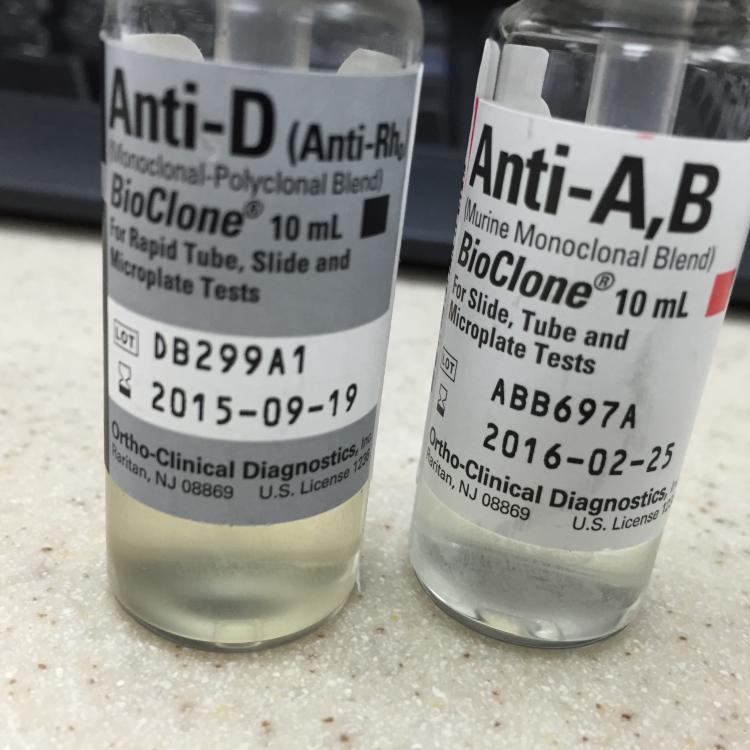
added sentence and edited sentenceWe use the ALBA-Q-Check QC vials. We add 40ul of ORTHO BioClone Anti-D to vial #4 to cause a positive DAT and a positive result in the Rh control test. See attached document of our daily QC results from ProVue. Our QC is designed to produce a positive and negative test result for each gel column in the A/B/D/R Monoclonal and Reverse Grouping card, the Anti-IgG Gel card, the A/B/D Monoclonal Grouping card, Buffered Gel card, SELECTOGEN, AFFIRMAGEN, MTS Diluent 2, and MTS Diluent 2+.
We do all our testing in ProVue including Type and Screen, Donor Unit Confirmations, Cord Blood testing, Weak D testing and both IgG and Buffered gel crossmatching and Antibody Identification.
-
32 minutes ago, 3cardmoe said:
Thanks for sharing this flowsheet. At the left hand bottom there is a box to document the elapsed time. What are your requirements for returning products? 30 minutes rule? If so, has your site 'validated' this rule?
This flowchart represents our requirements for handling blood components returned unused by Nursing.
There are three (3) basic elements: 1) Appearance, 2)Temperature, and 3) Time out of storage. If the visual inspection of the component does not reveal any unusual observation(s) and the component is within acceptable temperature limits and the component has not be out of storage for more than 30 minutes then the blood component may be reissued for transfusion.
1. Blood component is discarded if the container is spiked or outlet port(s) opened (regardless of temperature or time out of storage).
2. Blood component is discarded if the container contents are abnormal in color or appearance (regardless of temperature or time out of storage).
3. Blood component is discarded if the temperature of the blood component has exceed acceptable limits (regardless of appearance or time out of storage).
4. Blood component is discarded if more than 30 minutes has elapsed since removal from storage (regardless of appearance, temperature or time out of storage). We do not issue in coolers.
If any of the four (4) numbered statements above is/are true, component may not be reissued for transfusion and is immediately discarded into the biohazard trash. No exceptions.
The BBK CLS who receives a returned unit is required to complete this form and use a colored highlighter to trace his/her pathway from the starting point to a termination point. The completed form is reviewed by the supervisor and filed.
My understanding of the "30-minute" rule is that the temperature of component is ignored if the component has been out of storage for less than 30 minutes. We do not ignore temperature. There was an article in the AABB News several years ago that debunked the "30-minute" rule.
We borrowed our 30 minute time limit out of storage from the old rule, but did not validate. We assume that a blood component returned unused with a normal appearance, within temperature and within 30 minutes of issue may be reasonably returned to storage for reissue.
This process is intended to limit the number of decisions required to be made by a generalist.
-
-



contminated blood unit
in Transfusion Services
When the Transfusion Services becomes aware of such a situation, you have no choice but to demand unit be returned and discard it.