Content Type
Store
Profiles
Forums
Blogs
Events
Frequently Asked Questions
Gallery
Downloads
Glossary
Links Directory
Questions
Jobs
Vendors
Posts posted by Cliff
-
-
Many variables there, might be hard to compare.
We transfuse about 35k products a year and have a small donor center. We send FDA 50 - 75 reports a year.
-
Maybe try here?
-
3 hours ago, Micper81 said:
If anyone is interested, we have x 3 used Bio-Rad IH-1000 analyzers in excellent condition.
Michael
Michael,
Please stop posting ads in the forum.
Thanks
-
3 hours ago, Micper81 said:
If anyone is interested, we have x 3 used Bio-Rad IH-1000 for sale in an excellent condition.
These posts are not allowed here.
-
Correct Blood Bank Nomenclature
Correct Blood Bank Nomenclature
This question was submitted by forum member, Malcolm Needs. Any errors are those of the site admin, not Malcolm.
-
Submitter
-
Category
-
Submitted02/12/2018
-
-
-
I view the chart drive and digital display as electronic thermometers. When we used them in the distant past, we validated / calibrated them monthly. When we moved to Rees, they told us there monitoring devices were thermistors and are only required to be validated annually.
[Title 21, Volume 7] [Revised as of April 1, 2017] [CITE: 21CFR606.60]
TITLE 21--FOOD AND DRUGS CHAPTER I--FOOD AND DRUG ADMINISTRATION
DEPARTMENT OF HEALTH AND HUMAN SERVICESSUBCHAPTER F--BIOLOGICS PART 606 -- CURRENT GOOD MANUFACTURING PRACTICE FOR BLOOD AND BLOOD COMPONENTS
Subpart D--Equipment
Sec. 606.60 Equipment. (a) Equipment used in the collection, processing, compatibility testing, storage and distribution of blood and blood components shall be maintained in a clean and orderly manner and located so as to facilitate cleaning and maintenance. The equipment shall be observed, standardized and calibrated on a regularly scheduled basis as prescribed in the Standard Operating Procedures Manual and shall perform in the manner for which it was designed so as to assure compliance with the official requirements prescribed in this chapter for blood and blood products.
(b) Equipment that shall be observed, standardized and calibrated with at least the following frequency, include but are not limited to:
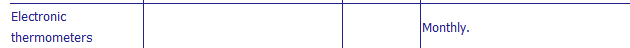
Equipment Performance check Frequency Frequency of calibration Temperature recorder Compare against thermometer Daily As necessary. Refrigerated centrifuge Observe speed and temperature Each day of use Do. Hematocrit centrifuge Standardize before initial use, after repairs or adjustments, and annually. Timer every 3 mo. General lab centrifuge Tachometer every 6 mo. Automated blood-typing machine Observe controls for correct results Each day of use Hemoglobinometer Standardize against cyanmethemoglobin standard ......do Refractometer Standardize against distilled water ......do Blood container scale Standardize against container of known weight ......do As necessary. Water bath Observe temperature ......do Do. Rh view box ......do ......do Do. Autoclave ......do Each time of use Do. Serologic rotators Observe controls for correct results Each day of use Speed as necessary. Laboratory thermometers Before initial use. Electronic thermometers Monthly. Vacuum blood agitator Observe weight of the first container of blood filled for correct results Each day of use Standardize with container of known mass or volume before initial use, and after repairs or adjustments. (c) Equipment employed in the sterilization of materials used in blood collection or for disposition of contaminated products shall be designed, maintained and utilized to ensure the destruction of contaminating microorganisms. The effectiveness of the sterilization procedure shall be no less than that achieved by an attained temperature of 121.5 deg. C (251 deg. F) maintained for 20 minutes by saturated steam or by an attained temperature of 170 deg. C (338 deg. F) maintained for 2 hours with dry heat.
[40 FR 53532, Nov. 18, 1975; 40 FR 55849, Dec. 2, 1975, as amended at 45 FR 9261, Feb. 12, 1980; 57 FR 11263, Apr. 2, 1992; 57 FR 12862, Apr. 13, 1992]
-
Antibody/Antigen Reaction
Antibody/Antigen Reaction
This question was submitted by forum member, Malcolm Needs. Any errors are those of the site admin, not Malcolm.
-
Submitter
-
Category
-
Submitted02/02/2018
-
-
Correct Blood Bank Nomenclature
This question was submitted by forum member, Malcolm Needs. Any errors are those of the site admin, not Malcolm.
-
Submitter
-
Category
-
Submitted01/15/2018
-
-
8 hours ago, Cliff said:
Can I ask why? If you are a huge facility and are trying to save money, you would make these from whole units. You'd have the resources to ensure they reagents are up to FDA requirements and the proper documentation was available for inspection. If your a small facility and are trying to save money, the few pennies you might save just aren't worth the regulatory risk.
If it's not money, what might it be?
Just curious.
-
Can I ask why? If you are a huge facility and are trying to save money, you would make these from whole units. You'd have the resources to ensure they reagents are up to FDA requirements and the proper documentation was available for inspection. If your a small facility and are trying to save money, the few pennies you might save just aren't worth the regulatory risk.
If not's not money, what might it be?
Just curious.
-
Welcome
-
Welcome
-
Ensure you use a vendor that uses an FDA approved adhesive. 21 CFR 175.105
-
It's mislabeled, so yes, it's reportable.
We are pretty big, and send in a lot of reports. The FDA is really easy to work with. I've had a couple of phone calls (they called me) and many emails regarding our reports. Again, always helpful.
-
Happy holidays to all.
-
3 hours ago, Mabel Adams said:
Keep thawed 5 day units on hand
This. We rarely outdate any.
-
7 hours ago, galvania said:
I didn't answer the question!!!!!!!!
Not even a week ago? Will the site let you try again? It's not supposed to.
-
Clinical Aspects of Transfusion Reactions
Clinical Aspects of Transfusion Reactions
This question was submitted by forum member, Malcolm Needs. Any errors are those of the site admin, not Malcolm.
-
Submitter
-
Category
-
Submitted12/11/2017
-
-
@SMILLER, we have always been able to determine who received our products, including all emergency release products. We have a form the physician signs that lists the units. The blood bank issues those products (when they have time) to that patient and we can track where every product goes.
What I take exception to is the inspector insisting that we also put the patients name and MRN on the product. They again insisted this made the process safer. It does not in any way make it safer, especially if it's a system assigned name / MRN and more importantly, when it takes a modest amount of time to generate these labels.
We have done a tremendous amount of planning to ensure we can give out emergency release coolers, almost on demand. It takes us very little time to give the requester their products, these labeled units have put a significant delay on that, and in my opinion, has deceased patient safety.
- jnadeau, TreeMoss, Malcolm Needs and 1 other
-
 4
4
-
7 hours ago, Malcolm Needs said:
I agree entirely Cliff, but, in the UK, largely as a result of The Blood Safety and Quality Regulations (BSQR), originally introduced in 2005 by the European Union (EU), we have to have an audit trail from vein to vein for all units of blood, blood components and blood products, and this is seen by the inspectors as MUCH more important than the mere life of a patient. Woe betide anyone who does not have a full audit trail and proof of cold chain, as they will have their finger nails ripped out without anaesthetic, then chucked into jail and the cell key thrown away. In other words, while I agree that there should be audit trails and cold chain proof, the attitude is totally over the top.
Yup, that was about how our inspection went. We were made to feel like we were murdering patients by not having a fake name, attached to a universally "safe" product, being infused into a exsanguinating, unidentified patient.
I understand the need for rules, but saving the patient comes first. We do have a trail of who got what. The idea that having a fake name on a product makes is safer is very frustrating.
-
As I mentioned, we need to go to a separate system just to print the labels to stick on to generic emergency release forms. All of this adds time. We are a large level 1 trauma center with a very active labor center. We have many emergency release situations. Some with dozens of products. This adds no safety at all and adds time; therefore in my humble opinion, decreases patient safety.
If I give an o neg RBC to the wrong patient (both of whom were going to get emergency released products), did I harm anyone?
-
We were cited last year for not labeling emergency release products. It was deemed an unsafe practice. Now we ask for the patients names and medical record number. If they don't have one, a temporary one is to be assigned and that info is provided to us. We then need to use a different system to print these stickers to place on the emergency release tags that we attach to the units. This can take a fair amount of time, but somehow is felt to be safer. Very frustrating.
-
Blood Transfusion Therapy in Haemoglobinopathies
Blood Transfusion Therapy in Haemoglobinopathies
This question was submitted by forum member, Malcolm Needs. Any errors are those of the site admin, not Malcolm.
-
Submitter
-
Category
-
Submitted11/13/2017
-



Pooled Cryoprecipitate
in Transfusion Services
Posted
We get ours pre-pooled from ARC. Far too much QC needed to do it in house. Also, I your LIS may not play well with a mixed ABO.