Posts posted by AMcCord
-
-
Can anyone give me the description for the CCP product - code E9804? The most current product code list I have for the ARC doesn't go there. I don't have a log in/access for the ICCBBA product code look up function.
Thanks!
-
-
22 hours ago, MAGNUM said:
Issueing a full unit for approximately 30 ml and discarding the rest is such a waste. Surely there is some other alternative.
Yes, it makes me sad to throw away the remainder of the unit.
But....the filter syringes have to be purchased by the case, which for us would be a near life-time supply and they are expensive to throw away every couple of years when almost all of them would be outdated. You have to demonstrate competency yearly for preparing aliquots and I don't know how you would do that without sacrificing units, plus for me to access competency when I would barely know what to do would be a joke. We would have to pay for the appropriate licensing yearly to relabel the syringes once split. We would have to have something like Digitrax set up and validated for use once or twice a year, because we don't need to relabel anything else. Our blood center is 150 miles away so its not feasible to order blood in pedi-packs for urgent need. I don't feel that stocking units like that for use once or twice a year makes good sense. I doubt that our supply would agree to do it anyway. My BB LIS isn't set up to receive or use splits, so more validation. Once I split the unit, the remainder of the unit would have to be transfused within 24 hours because we don't have sterile docking capability - more money, more competencies. We do actually have a day now and then when no one is transfused, so the remaining part of the unit might still be wasted.
I've run this scenario through my head multiple times and I've never come up with a better option than handing over an entire unit to be used as the provider requires. Still makes me sad to discard the unit.
-
On 11/5/2018 at 8:20 AM, R1R2 said:
I would think that the freshest irradiated or unirradiated unit you have on hand would be suitable for a baby in a true emergency. A full unit could be issued and tranfusionist would use what they needed and discard. This plan should be discussed with all involved before it happens to make sure everyone is OK with this. Perhaps a procedure should be written as well.
This is the plan we use for the 1 -2 units we transfuse to infants each year.
-
-
-
-
Edited by AMcCord
On 9/29/2020 at 8:58 AM, Sonya Martinez said:On 9/25/2020 at 8:45 AM, DebbieL said:I know when CAP revived the standard, I was upset because I also thought I had to revert back to ice and water to make the chart move on my Helmer fridges and PLT incubator during alarm checks. That was moving backward as far as i was concerned.
I called Helmer and finally received a PDF regarding Helmer and TRM.42750. I was also sending email questions to CAP at the same time. Our equipment is older and doesn't have printouts but CAP stated a photo of when the alarm sounded should be OK to proof. (I am keeping that email for a future inspection, just in case.) I take a photo of the electronic screen showing the temp at which the alarm sounded and add to my Alarm Check QC sheets.
202001 TRM.42750 Helmer Solution for Alarm Checks.pdf 2.22 MB · 65 downloads
Bless you for sharing!!!
-
On 10/2/2020 at 8:06 AM, DebbieL said:
Sonya Martinez- You are welcome! I was horrified that we had to revert back to messy ice and thermometers when we paid extra for the Helmer alarm system.
If you figure out how to "map" a fridge, please share with the rest of us. I would guess sticking thermometers all over to see where the warm spots are located but who knows.
I Googled it and found procedures for pharmaceutical industry use that were very detailed/rigid that would require me to monitor 9 locations in my two door fridge and 5 in my one door fridge. I discussed this with someone who is familiar with this sort of thing. He suggested that it would be adequate to monitor 4 temp points in a two door blood storage refrigerator - top left rear, bottom left front, top right front, bottom right rear. He feels that I can use historical data to document that the refrigerators in use have been monitored and are operating within appropriate limits. I have checked multiple temps/multiple locations and documented that after installation of the units (years ago) and after repairs so I can prove that the temps have been consistent throughout the life of the units. I can state that I have been monitoring multiple temps ( two bottles and two built in probes) in different locations in the refrigerator daily (top, bottom and center) and historically those temps have matched + 1 C daily as specified by SOP.
Going forward, we will need to map after repairs and when replacing refrigerators. I think I'll go ahead and do that now when I get a chance just to see what the data looks like. I will use inexpensive data loggers so I can collect multiple data points over multiple days. Once that is complete I will know where to best place the thermometer bottles I'm currently using (two of them) to make sure they are in the hot and cold spots. I needed a new project - nothing better to do
 .
.
-
-
Edited by AMcCord
Yes, our medical director signs off on major revisions/new forms. We also use MediaLab.
My current struggle is making staff understand that they may NOT copy copies of forms but must print them from MediaLab
 . Apparently signing in to MediaLab is too 'inconvenient' because they have to sign into their email first
. Apparently signing in to MediaLab is too 'inconvenient' because they have to sign into their email first  .?. Sigh...
.?. Sigh...
-
If the same sample is used for both types, CAP does not require a different tech to perform the second type. CAP doesn't require a second sample drawn by a different person for transfusions. You can meet the requirement for mitigating misidentification risk by utilizing an electronic ID verification system at the bedside when specimens are collected and by using a mechanical barrier system for patient ID/unit ID when transfused. Verifying the ABO group with a second sample is another option.
-
-
Hand held ID devices are great. We use them. But...they are only as good as the patient ID process when that individual is admitted and banded in the first place. Or rebanded because they have removed an ID bracelet. Lab has detected some of those cases. That uncertainty leads us to use a blood bank band with a physical barrier for blood product transfusions.
-
I do as David does - a note to indicate that the patient is a Jehovah's Witness. If the patient has accepted plasma but not red cells, I will also note that. Saves them a bill for an unwanted crossmatch sometimes if I can notify the provider that he/she should discuss transfusion with the patient before we perform testing to set up red cells for them. (And yes, I think that providers should discuss transfusion with their patients, ideally before ordering the products, but we know that the real world doesn't always work that way.)
-
On 8/21/2020 at 6:07 AM, exlimey said:
That's an excellent point. It always struck me as slightly odd that such critical testing is done by "drops" - a potentially highly variable volume. One certainly wouldn't see an HIV test kit give instructions like "Dispense two drops". Goes to show that the standard serological (tube) test is extremely tolerant of variation.
True, but I suppose we can also say that there has been years and years worth of testing performed that way with no evidence of harm reported from the practice.
-
-
-
21 hours ago, exlimey said:
Wow. I perfectly understand the science, but that is an awful thing to put in a Directions for Use. A savvy Inspector could throw serious doubt on any tests performed using the supplied dropper. And why provide a dropper if it isn't good enough for the test ? The only way to meet this requirement to the fullest is to use a calibrated semiautomatic pipette.
Or is the question the quality of the disposable pipette that is used for the patient plasma? We do use a disposable intended for Blood Bank use with a statement on the box 'consistent drop size'. I would say that you could present documentation that you've verified volume delivered (on average - since its a disposable) by the pipette vs the dropper in the vial.
-
21 hours ago, David Saikin said:
Also, a few years ago the FDA was considering having BBs file for lab developed tests if you used any enhancement media, even though you were following the pkg inserts. If you used more than saline and serum you could file for a lab developed test with no surcharge ($250,000) up until a designated date. After that date you would have to pay. I have not heard that they were pursuing this any longer. That surcharge is what vendors have to pay initially to have their product evaluated for FDA approval (or so I understand).
I would hope that someone has convinced them that this is a crazy thought.
-
-
Edited by AMcCord
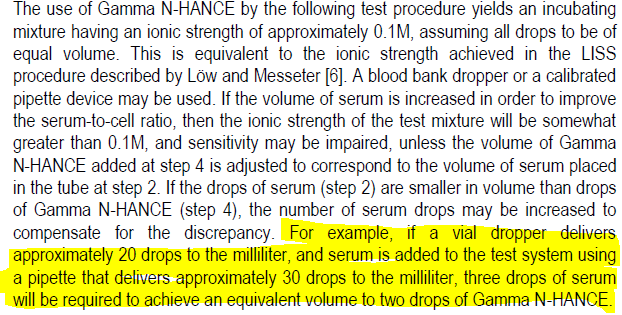
2 hours ago, Monique said:We switched to N-Hance years ago in order to comply with Massachusetts Water Resources regulations. ImmuAdd contains the preservative thimerosol-a mercury contaminant. We performed a small validation and found that N-Hance performed as well as ImmuAdd. Only one problem: the manufacturer's insert suggests using a transfer pipet to dispense the additive rather than the vial dropper in order to maintain the proper ionic strength. When we open a vial, we always discard the dropper and replace it with a stopper.
For reference:
-
-


Covid Convalescent Plasma Product Code Description
in Transfusion Services
Thank you! I knew I could count on this group.