Posts posted by exlimey
-
-
On 2/19/2021 at 4:09 PM, diplomatic_scarf said:
I disagree. Most gel cards and Anti-D reagents won't detect DVI for patients. Fortunately I can find numerous suitable quotes, because it's true.
https://labs-inc.org/pdf/361_3.pdf
Apologies. I was discussing reagents used in tubes, not gel cards.
-
On 2/17/2021 at 3:43 PM, diplomatic_scarf said:
"Modern anti-D reagents, while they are very good at detecting weaker forms of the D antigen, are specifically designed to NOT detect the most common form of partial D in Caucasians (DVI, or “D six”), so most Caucasian partial D patients will test as D-negative." -BloodBank Guy
https://www.bbguy.org/education/glossary/glp04/
I disagree. It is in the FDA's manufacturing requirements that DVI be detected. Unfortunately, I couldn't find a suitable CFR quote, but several of the Directions for Use I looked at from different manufacturers indicate that they detect DVI.
However, I agree that strategic differential use of reagents such as these on patients vs donors can certainly help the transfusionist and/or determine the necessity for Rh Immune globulin.
-
14 hours ago, diplomatic_scarf said:
I think most modern Anti-D reagents won't detect DVI and these patients will test as D-negative. This is probably the answer. Anyways, this is the answer he gave his students. To me, the answer looks as vague as the question. Not "straight forward" at all.
IMG_2756.heic 2.45 MB · 4 downloads
Anti-D reagents are specifically formulated to detect DVI - that is REQUIRED by the FDA in the USA. It was also true of the human sera-based reagents I manufactured in the UK during the 1980s.
There was a period when anti-D reagents were approved for donors or patients. The reagents used for donors were required to detect DVI, arguably the "weakest" expression of the D antigen of the known D-variant and typically that meant an antiglobulin phase was required. Those reagents formulated for patients often were not designed to detect DVI (had no IAT) and subscribed to the "it's better to treat them as D-" philosophy.
Today's reagents are typically qualified/licensed for patients and donors, i.e., they are formulated with the same performance characteristics. Even so, all are a blend of monoclonals (IgM/IgG) since not one single clone can detect all of the "normal variants" (a great oxymoron).
Apologies for some of the antiquated terminology.
-
-
-
-
18 hours ago, Malcolm Needs said:
I, too, am DCe/DCe (R1R1). This is getting spooky! Maybe you are on to something exlimey, and should write it up for Vox Sanguinis, Transfusion and/or Transfusion Medicine, or maybe even Nature!
An interesting idea, but I'm not sure I want my psychological dirty laundry hung out for the world to see.

-
1 hour ago, Malcolm Needs said:
Ah, but don't forget that, not only did I work in a Reference Laboratory, but am also a self-confessed pedant, and so, if a patient was both c Negative and E Negative, and had an anti-c, we would go to the ends of the Earth to prove the presence or absence of an anti-E, as a matter of pride!





I confess: I'm much the same way in the OCD sense. I'm also DCeDCe (R1R1), so perhaps this issue hits a little too close to the sensitive area.

-
23 hours ago, John C. Staley said:
Couple of more strange questions, how sure are you that it is anti-Jka? If you are sure, why were you doing a ficin panel?
Can't wait to see what Malcolm has to say.

An EXCELLENT question, John, but as Malcolm suggests, is appears that there is still a large dose of "we always do that" in many laboratories.
-
Short answer: Yes
How was the anti-Jka detected initially, i.e., what technique ? Assuming it was an antiglobulin test, but was it Gel, Solid Phase, LISS, PEG ?
Yes, the panel cells are now ficin-treated and antibodies to Jka should be enhanced, but the test conditions that were used in the original assay may not exist when ficin-treated cells are used - one may need to add LISS or PEG, one may need to test by Gel or Solid Phase.
-
-
2 hours ago, Joanne P. Scannell said:
However, things do happen and I agree with exlimely, if you do have to change or replace (say it fell out for some reason) a battery, then a 'calibration' would be prudent.
Also, we are not talking high precision here, i.e. wider acceptability range than a pipette would be, i.e. testing is done in ranges of time, not exact seconds. This 'calibration' is just a simple check up to make sure the timer isn't totally out of range. Most of the time, the error is the readout gets 'broken', not the accuracy of the timer.
Actually, I'm not suggesting that replacement of the batteries is cause to re-qualify a timer. Accuracy of most timers is not affected by battery replacement because there is no actual CALIBRATION, i.e., no adjustment process. Typically, today's timers are CERTIFIED - their accuracy is verified against a standard. That accuracy is independent of the batteries.
But, I do agree that a broken/unreadable timer is the ultimate expression of "inaccurate".

-
Perhaps the real question is: Do you (or the supplier/certifier) actually CALIBRATE them ? That is, can the reading be adjusted in any way ? If the timer differs greatly from the "Standard", can it be tweaked into range ? Most simple electronic (battery-powered) timers are not adjustable. I'm not even sure that the official certifiers (the ones providing the certificates) are able to adjust the cheap and cheerful electronic timers. The electronics are so reliable (and cheap) these days that it's rare to find an inaccurate timer. The ones with unacceptable performance are probably just discarded.
So, back the the main issue. If the time IS calibrated and the removal of the batteries nullifies that calibration, i.e., the timer loses its mind, then YES, the timer will need recalibration upon battery replacement. But, see above, I suspect not.
-
Tests on the adsorbed serum (with ZZAP-treated cells) give confidence that the are no underlying alloantibodies to common antigens. However, the use of allogeneic cells risks removal of a cold-reactive alloantibody to a high incidence antigen, e.g. anti-Vel, -PP1pK. A low risk, but still concerning.
Does you facility also test the ZZAP-treated patient cells (now presumably DAT-negative) back against the patient's own serum ? This is ultimate proof that the cold-reactive antibody is an AUTOantibody and adds more confidence in the results of the adsorption with allogenic cells.
I may be opening a can of worms here, but.....I question the use of ZZAP in this scenario. In this case, the adsorption used (presumably DAT-negative) allogenic cells. ZZAP was not required to "reduce the DAT and enhance antibody uptake" - which is a true statement about performing AUTOadsorptions with DAT-positive cells. I appreciate that the enzyme in ZZAP enhances the efficiency of the adsorption, but the DTT component is not necessary for most alloadsorptions, and can actually confuse the users. I suspect the answer/policy is related to ZZAP being commercially available, rather than in a well-founded technical reason.
-
15 hours ago, Blood Bank student said:
Hi,
We had a grouping discrepancy for a patient where forward group reactions were all positive including the Rh control.
Patient's original group was A positive but we had weak reactions with Anti-A and A1 cells.
(washed patient cells 4 times with RT saline and repeated group, same reactions)
The antibody screen was positive including the autocontrol. Dat and eluate all positive. So we thought it's a warm auto and send it to our reference lab for investigation.
They performed adsorption with zzap'd cells and there was no clinically significant antibody detected in adsorbed plasma.
To resolve the grouping discrepancy they used prewarm technique and got a valid ABO.
My question is about the use of this pre-warming technique to resolve the grouping discrepancy. Was it appropriate to resolve the group without proving the presence of a cold antibody?
Thank you
Arguably the initial ABO discrepancy is proof of the presence of a cold-reactive antibody.
If the DAT was positive, how do you determine that the autocontrol is valid ? Surely its just the same DAT-positive cells reacting with the antiglobulin reagent, or were the patient's cells treated to render them DAT-negative prior to testing ?
Were the "zzap'd cells" autologous ?
-
-
22 hours ago, AMcCord said:
Or is the question the quality of the disposable pipette that is used for the patient plasma? We do use a disposable intended for Blood Bank use with a statement on the box 'consistent drop size'. I would say that you could present documentation that you've verified volume delivered (on average - since its a disposable) by the pipette vs the dropper in the vial.
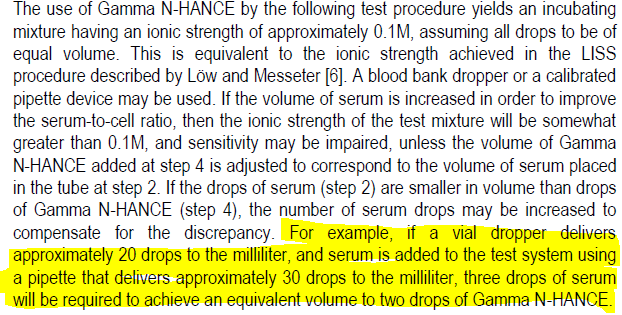
That's an excellent point. It always struck me as slightly odd that such critical testing is done by "drops" - a potentially highly variable volume. One certainly wouldn't see an HIV test kit give instructions like "Dispense two drops". Goes to show that the standard serological (tube) test is extremely tolerant of variation.
-
2 hours ago, AMcCord said:
Wow. I perfectly understand the science, but that is an awful thing to put in a Directions for Use. A savvy Inspector could throw serious doubt on any tests performed using the supplied dropper. And why provide a dropper if it isn't good enough for the test ? The only way to meet this requirement to the fullest is to use a calibrated semiautomatic pipette.
-
18 minutes ago, e specificity said:
We had a situation with discordant/variable little s typings (but caucasian) and genotyping came back without flags as little s+. In the end, the patient had a glycophorin hybrid that required sequencing to determine with an antibody classified as anti-Ena.
Eek ! I hope they don't need transfusion.
-
On 7/31/2020 at 4:42 PM, Blood_Banker said:
Thanks. Finally found a great journal article about this phenomena - just takes googling the right keywords to find something. Here is a link for those interested.
https://onlinelibrary.wiley.com/doi/full/10.1111/vox.12909
Oops. Perhaps "Mia" is not as obsolete as I believed.
 Great article/reference.
Great article/reference.
-
Yes. In the examples I've seen, the usual the culprit is a gene re-arrangement that results in expression of the Dantu antigen. If I remember correctly, the P3BER clone does not react with Dantu+ cells. If it isn't mentioned in the Directions for Use, you could check with the technical people at Millipore/Bioscot.
The presence of "Mia" (an obsolete umbrella term that can apply several "Miltenberger" antigens), already indicates that some MNS gene shuffling has occurred.
-
-
2 hours ago, jayinsat said:
I would suggest running a select panel of low-frequency antigens against your patient's plasma (V, Cw, Jsa, Kpa, LUa, Bga, Ch, etc). If the patient has one of those antibodies, the antibody screen would still be negative and, likely, so would your panel if there is no positive cell included. The unit may have the corresponding antigen. I have seen this several times. Since we don't routinely do serological crossmatches in the presence of a negative antibody screen, these antibodies are normally not found until a transfusion reaction investigation.
This scenario doesn't explain why the donor red cells react with the serum from most patients. For this to be a "low incidence antigen" issue, ALL of the patients would have to have an antibody to (probably) the same low incidence antigen. That is very unlikely. As Malcolm suggests, this sounds like an abnormality of the donor's red cells.
I believe Hemo bioscience have a lectin kit, but it may only be available in the USA.
-
19 hours ago, Malcolm Needs said:
I can't refresh your memory, but I do know of a case of anti-Vel in the UK that caused a fatal transfusion reaction. The DAT was positive by anti-complement only, and the anti-Vel itself could only be detected in a clotted sample, not in an EDTA sample.
Those anti-Vels are sneaky !




Micro only reactions
in Transfusion Services
I was originally trained using an "inverted microscope" - that was a thing of beauty. The light source was above, the relatively low-powered lens below. The cells stayed in the tube and the tube could be rotated to get movement and/or a suitable thickness of liquid in which to see the cells. It was great and very easy to use (even though it had a large footprint), but as others have commented, if one looked long enough, one could always find "friendly cells".
I'm not a fan of microscopic reading and I dissuade others from doing it. As I've said in the past, high level tools and techniques should only be employed by those who understand the limitations and consequences.