Content Type
Store
Profiles
Forums
Blogs
Events
Frequently Asked Questions
Gallery
Downloads
Glossary
Links Directory
Questions
Jobs
Vendors
Posts posted by Eagle Eye
-
-
Same here. I run one Positive and one negative for all tests.
-
If you use a diluted 3% panel for routine gel testing and want to validate it's performance/stability for 1 week...How many days or specimens would be required?
Please check manufacturer package insert. I know Ortho insert is 24 hrs. If you are extending days against package insert, you should validate with all kind of specimens and include worst cases. And definetly, you should run every day and in parallel with reagent prepared per package insert.
Eg. you can run X number of specimens (Pos and Neg) with freshly diluted cells (up to 24 hrs expiration) and diluted cells you are trying to validate. Make sure to document reaction strength and any missed reaction. I would try to make sure there is no variability in procedure. (tech to tech variation).
-
infared Raytek ----anyone can share make and model#?
-
Are you happy with Tempcheck? we have it in box for four years as our initial validation was not acceptable!
-
Anyone is using infrared thermometer to take temperature of returned units?
Do you get reproducible reading?
How do you take temperature? DO you have procedure you can share?
How often do you send it for calibration?
Make and model of the thermometer in use please?
-
On 2/22/2018 at 2:20 PM, Eman said:
I guess I could clarify that our validation environment (and training environment) is identical to the live production environment, except the "other" two environments don't interface to billing.
We have the same BUT we decided to use production as what if!...
It is very easy to block billing by just creating a code at interface level.
We also use teo patient to stock in ER and OR and again we hav eit blocked at interface so it does not generate any transactions.
-
Any one using Monoclonal Control (immucor reagent ) when performing weak D test or for AB Pos CORD.
Are you using one drop or two drop of monoclonal control.
-
How do you document manual entry verification?
I know someone had shared their SOP here but i can not find it...please help.
-
You know what i had brain block!!
I was thinking about digital/electronic timer....and panicked as we validate them every six month.....Oh thank GOD!
-
On 1/29/2018 at 1:04 PM, Eman said:
Doesn't seem extreme to us at all, we also enter PT specimens into our LIS, although we use the validation environment to keep fake patients out of the live side, which also means we don't get billing issues with these. By managing the PT specimens in the LIS we are truly treating them like real patient specimens.
We use production as we wanted to mimic real patient. Only difference...the order is not coming from EPIC. we record specimen in safetrace.
We use same last name all the time and we have it blocked at interface level so billing is not generated.
-
Ortho is good at adding revison summary.
Immucor---says they will underline and tringle....many times there is a change in their address and which is not underline so original poster's frustration is right.
I went through same and at the end noticed that the immucor address was chagned which was nor underline...
-
On 2/2/2018 at 7:12 AM, Cliff said:
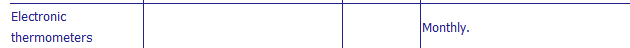
I view the chart drive and digital display as electronic thermometers. When we used them in the distant past, we validated / calibrated them monthly. When we moved to Rees, they told us there monitoring devices were thermistors and are only required to be validated annually.
[Title 21, Volume 7] [Revised as of April 1, 2017] [CITE: 21CFR606.60] TITLE 21--FOOD AND DRUGS CHAPTER I--FOOD AND DRUG ADMINISTRATION
DEPARTMENT OF HEALTH AND HUMAN SERVICESSUBCHAPTER F--BIOLOGICS PART 606 -- CURRENT GOOD MANUFACTURING PRACTICE FOR BLOOD AND BLOOD COMPONENTS
Subpart D--Equipment
Sec. 606.60 Equipment. (a) Equipment used in the collection, processing, compatibility testing, storage and distribution of blood and blood components shall be maintained in a clean and orderly manner and located so as to facilitate cleaning and maintenance. The equipment shall be observed, standardized and calibrated on a regularly scheduled basis as prescribed in the Standard Operating Procedures Manual and shall perform in the manner for which it was designed so as to assure compliance with the official requirements prescribed in this chapter for blood and blood products.
(b) Equipment that shall be observed, standardized and calibrated with at least the following frequency, include but are not limited to:
Equipment Performance check Frequency Frequency of calibration Temperature recorder Compare against thermometer Daily As necessary. Refrigerated centrifuge Observe speed and temperature Each day of use Do. Hematocrit centrifuge Standardize before initial use, after repairs or adjustments, and annually. Timer every 3 mo. General lab centrifuge Tachometer every 6 mo. Automated blood-typing machine Observe controls for correct results Each day of use Hemoglobinometer Standardize against cyanmethemoglobin standard ......do Refractometer Standardize against distilled water ......do Blood container scale Standardize against container of known weight ......do As necessary. Water bath Observe temperature ......do Do. Rh view box ......do ......do Do. Autoclave ......do Each time of use Do. Serologic rotators Observe controls for correct results Each day of use Speed as necessary. Laboratory thermometers Before initial use. Electronic thermometers Monthly. Vacuum blood agitator Observe weight of the first container of blood filled for correct results Each day of use Standardize with container of known mass or volume before initial use, and after repairs or adjustments. (c) Equipment employed in the sterilization of materials used in blood collection or for disposition of contaminated products shall be designed, maintained and utilized to ensure the destruction of contaminating microorganisms. The effectiveness of the sterilization procedure shall be no less than that achieved by an attained temperature of 121.5 deg. C (251 deg. F) maintained for 20 minutes by saturated steam or by an attained temperature of 170 deg. C (338 deg. F) maintained for 2 hours with dry heat.
[40 FR 53532, Nov. 18, 1975; 40 FR 55849, Dec. 2, 1975, as amended at 45 FR 9261, Feb. 12, 1980; 57 FR 11263, Apr. 2, 1992; 57 FR 12862, Apr. 13, 1992]

Do you calibrate your digital thermometer monthly?
-
I just answered this question.
-
My ScoreFAIL
-
-
For method correlation: only two sample. one positive and negative. Usually postive has one of two antibodies.
Initial validation was done many years ago but if i have to do it now, i will do total 20 specimens and at least five or more positive with different antibodies (Anti-E, anti-K, ANti-D due to RHogam, warm auto and atleast one example of cold antibody)
-
Yes. If you combine plasma and red blood cells in your blood bank you need to register with FDA and be ready for FDA inspections!
-
I just answered this question.
-
My ScorePASS
-
-
1) Think about taking the exam without the online course.
2) I had less than two years BB experience and was new QA position and took online course....lots of work but as suggested earlier in the post you have to have a set schedule...3-4 hours daily dedicated for this...you can do it.
-
We do the same. Register all CAP specimens as patients and donor as blood unit and just treat like actual patient.
You might want to think about using your LIS as corrective action to prevent the error in future.
Do you have second tech verifying your gel card readings?
All our manual gel results are co-signed by second tech.
-
It really helps a ton if you are getting your specimens ASAP for massive transfusion protocol. It avoids using AB plasma or low titer A plasma...
-
We include a step in our method corelation (twice a year) where we run Ortho gel panel (0.8%), Tube panel (immucor 3%) and Immucor gel panel(dilute immucor to 0.8%). Our method was correlated almost 20 years ago!
- MOBB and Carrie Easley
-
 2
2
-
physician responsibility
-
On 1/21/2018 at 3:58 PM, mollyredone said:
Do you have Meditech? I saw a place I could print a list putting in specific antigen typings, but it prints one page for each antigen and blood type. Kind of tedious.
we have safetrace and you can search by antigen and/or blood type. for multiple antigens you can specify if you want to see unit negative for all antigens or some!
-
All my techs when in training they are not to enter any patient result in system until training is completed and they are competent. (Passed competency).
-
I just answered this question.
-
My ScoreFAIL
-



Adult DAT's and antigen typing on the Ortho Vision
in Transfusion Services
Posted
We do not have vision but we have been using antigen typing cards ...for many years. It is very simple and tech likes it and less human steps less errors. We require our techs to cut the segments instead of using segment devise to make sure we have enough cells/packed cells to run test.