Posts posted by Kelly Guenthner
-
-
50 minutes ago, kjmiller said: We still do all their testing because they do not have their own blood bank, but when we result the type and screen, we do it under their hospital ID in the LIS (Sunquest). The problem is that if one of their patient is now transfered to our facility for a higher level of care, we are having to rearmband, redraw, and retest the patient - just as if they had come from any other hospital.
I think this is the key: Is initial testing at that ED is under one patient identifier/armband and the testing at your facility under a completely different patient identifier/armband?
It's less about the testing, more about the patient identification.
From CAP:
TRM.40230
Specimen Labeling for Pretransfusion Testing
Phase II
All blood samples used for pretransfusion testing are labeled at the time of specimen collection in the presence of the patient with:
1. Patient's first and last name
2. Unique identification number
3. Date of collection
4. A method to identify the individual collecting the specimen.
NOTE: Blood specimens collected for pretransfusion testing must be positively and completely identified and labeled before leaving the patient. Acceptable practices for positive identification of patient and blood specimen labels must be defined in the procedure manual and may include visual inspection and/or an electronic system to read the identifying information contained in bar codes or radio-frequency identification (RFID) microchips or the patient's wristband. Acceptable practices for generating specimen labels must be defined in the procedure manual (refer to GEN.40490) and may include electronic devices utilizing information encoded in bar codes or RFID microchips. There must be a dependable method to identify the individual who collected the blood specimen, such as initials or another identifier on the tube, or an electronic record.
Evidence of Compliance
✓ Properly labeled blood specimens AND
✓ Records identifying the individual collecting pretransfusion testing specimens
-
We use a hands-off process where the floor faxes their request for blood, the blood banker sends the unit via the pneumatic tube and the floor faxes/sends back the signed copy of the unit tag.
I am finding it difficult to come up with a routine transfusion scenario that does not involve 2 people at issue (one on the floor, one in the blood bank).
I can come up with a couple of CAP requirements that you could cite, though they don't explicitly say 2 people at issue, you could certainly argue that your way of satisfying the requirement is to have one person from the floor, one person in the blood bank at issue.
-
On 1/27/2025 at 11:22 AM, kab1 said:
Hi all, perhaps this is a silly question. We are a growing blood bank that works primarily in gel. We only ever have 2 available panels to use at a time, Ortho Panel A and Panel B. We are bringing in a tube panel to use as an additional resource (Immucor/Werfen Panocell). My question is, if we are working up an antibody ID in gel and need additional rule-outs, can we use selected cells from the tube panel (using tube testing method) to complete our workup? Can you piece together gel and tube to support one antibody ID? I cannot find any guidance on this in the technical manual, any insight is appreciated. Thanks in advance!
We use Ortho Panel A (gel) as our primary method; Immucor/Werfen panocell as supplement (diluting to 0.8% and using gel; will also use PEG/LISS IAT as warranted). Additionally, we save a couple months worth of expired cells to use for selected cells, when our in-dated cells don't have the right antigen combo.
-
On 11/22/2024 at 10:34 AM, Darcy said:
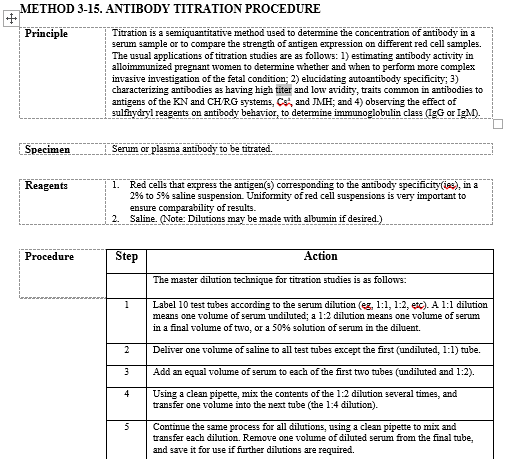
Have there been any updates to titer QC since these posts? We have an upcoming inspection next year, and we were told that we should be running QC for titers. Currently we do previous and current specimens in Gel on the Vision. Any standardized QC produced by suppliers? I would think the simplest and / or easiest to produce ourselves would be some kind of Anti-D value. Any suggestions?
We also do titers on the Vision. We keep an aliquot of the previous titer, but only test it in parallel with the current if there is a significant difference to the current (titer jumps/drops 2 or more dilutions [The increase of 2 or more is our alert/critical value]).
We titer against screen cells, which are QC'd daily and do not do any additional titer QC.
-
1 hour ago, Andrea Pointer said:
Discarding your tips is a "best practice" from molecular assay pipetting techniques (my work history is in molec genetics before I went to BB). It may truly not make a difference on the macro scale for most blood banking, but we opted to retain the practice of fresh tips to avoid any potential carryover.
Discarding your tips is also the AABB standard practice:
-
-
-
21 hours ago, LK11 said:
Current workflow: The first Type and Screen ordered/resulted has an outdate of expiring on the 3rd day (after collection) at midnight. All product orders will net to this Type and Screen order. A new Type and Screen order is allowed in on the 3rd day after 12pm.
Duplicate Type and Screen ordered in Epic 'net' into the same Soft order, but label does not print for a new collection. This keeps any product orders on the active T&S sample.
3 minutes ago, jshepherd said:When a sample is drawn before midnight on the third day, we have to manually go in and inactivate/expire the existing TYSC sample so that product orders will flow onto the new TYSC.
We function with your current workflow description and @jshepherd's work-around description.
-
-
Edited by Kelly Guenthner
Our prenatal TS come from outside clinics and are registered with outside referral medical record numbers that are different from the hospital medical record numbers (under which they would be transfused). Because they are immunohematology
 and not pre-transfusion, we do not require a second ABORH.
and not pre-transfusion, we do not require a second ABORH.
Prenatal referral records will be linked to hospital records, but the ABORH will not count as a second type on record in transfusion situations.
-
Edited by Kelly Guenthner
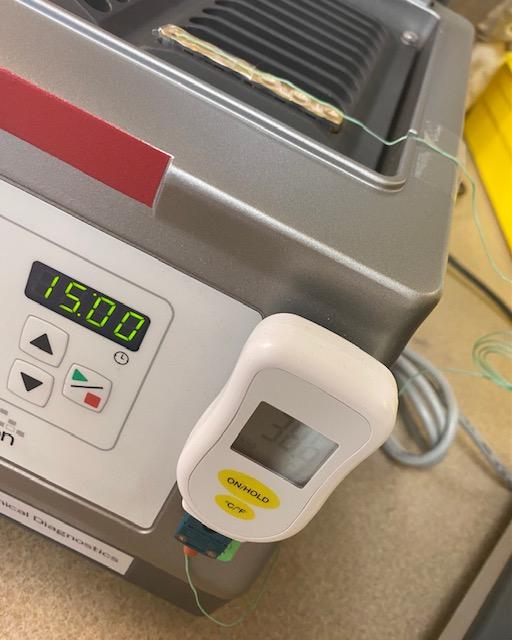
From the CAP Transfusion Medicine Checklist:
COMPONENT PREPARATION, STORAGE AND MODIFICATION
The following component definitions are offered as a convenience:
Component
Definition
Fresh Frozen Plasma (FFP)
Plasma frozen within 8 hours of collection after being separated from a unit of whole blood or frozen within 6 hours after collection by apheresis
Plasma Frozen Within 24 Hours After Phlebotomy
Plasma separated from whole blood and frozen between 8-24 hours after collection
FFP, Thawed
Fresh Frozen Plasma thawed between 30-37°C, then stored at 1-6°C for up to 24 hours
Plasma Frozen Within 24 Hours After Phlebotomy, Thawed
Plasma frozen within 24 hours of collection that has been thawed between 30-37°C, then stored at 1-6°C for up to 24 hours
Thawed Plasma
“FFP, Thawed” or “Plasma Frozen Within 24 hours After Phlebotomy, Thawed” which is stored in a closed system at 1-6°C for 1-5 days after thawing
and the related standard:
TRM.44525
Thawed Plasma Label
Phase II
If Fresh Frozen Plasma or plasma frozen within 24 hours of collection is thawed at 30 to 37°C and maintained at 1 to 6°C for one to five days, it is relabeled as "Thawed Plasma".
My interpretation is only Thawed Plasma, (either FFP or FP24), stored >24 hours (1-5 days) requires relabeling.
-
-
-
Edited by Kelly Guenthner
55 minutes ago, jshepherd said:Must you have the temp indicators?
Not the original poster, but we use them in coolers to the OR and shipping boxes we send to outlying clients. An electronic data logger accompanies units in the cooler to ensure the cooler has remained at temp; Safe-T-Vue ensures that the unit has remained at temp. In our shipping boxes, clients have the option of using the Safe-T-Vue as the sole indicator; though most back it up with a temp gun/thermometer reading on arrival.
We're going to stick with Safe-T-Vue, despite the price jump.
-
-
On 1/9/2024 at 2:29 PM, Cliff said:
Is it this one?
https://packmaxq.com/product/maxplus-blood-coolers/
The handle looks rather specific and integrated. That might be hard to replace.
Have you talked with your Biomed folks? Often, they can work miracles.

That's the one! And the handle is integrated, but has 2 little screws that allow it to be removed the rest of the integrated assembly. Should be an easy replacement, once we find a match! (We're doing the legwork on this particular project, as our Biomed is very busy!)
-
Has anyone successfully replaced the telescoping luggage handles on their MaxQ coolers, either with manufacturer provided replacements or "after-market" parts (Amazon?)?
We have been using (and loving) our MaxQ coolers for about 4.5 years now. so much so that we've banged up the telescoping luggage handles pretty good.
When querying the manufacturer about replacing the handles, they say "Nope! Gotta replace the whole box!"
-
On 4/4/2023 at 8:07 AM, jayinsat said:
Question: why are you looking for glass pipettes? We were forced to stop using glass pipettes years ago by our infection control team (glass breakage/employee injury risk). We were able to keep the glass tubes because of the potential effect on antibody detection. I do not believe using plastic pipettes pose any risk though.
Not looking for glass, per se... but, we had still been using traditional soda lime blood bank pipettes You know... because... "That's what we always use!"
 . I guess no one here cares about safety!
. I guess no one here cares about safety! 
When we ran into manufacturing shortages of those, we used up the leftover glass borosilicate pipettes from the core lab. Now, we're on to plastic (Cardinal CH5214-12 or CHB521412), which is probably what we'll stick with.
Thanks for your input, everyone!
-
I believe OP is referring to this publication:

-
Well, I feel like a real dope for asking, but, what pipettes are y'all using for your bench testing, these days?
My purchasing coordinator is at her absolute wits-end trying to find blood bank suitable pipettes. She has orders in to every manufacturer imaginable for standard blood bank soda lime glass pipettes. Additionally, we've seemingly burned through every available stash of borosilicate glass pipettes she can get her hands on. We've now moved on to the smallest available plastic transfer pipettes (that still deliver a standard blood bank-sized drop), but may need to switch to larger transfer pipettes!
Anyone have a source they want to share?

-
-
-
-



Standard regarding sharing of pre-transfusion testing results between hospitals
in Accrediting Agencies
Your policy (to draw and test your own specimen) is the strictest interpretation of the standards (and one that most blood banks likely follow), but I do believe you'll find systems that share MRNs, share LIS, share policy & procedure (may even share technical staff) that will use pretransfusion results performed in blood bank A to transfuse the patient at location B by technical staff in blood bank B and are doing so within AABB and CAP standards.
All that is to say, I don't think you'll find a standard that explicitly says you have to draw and test your own specimen at your own physical location. We come to that conclusion because of all the other standards.