-
General Lab: Dilution
I just answered this question. My Score PASS
-
-
-
 Emelie reacted to a post in a topic:
Why irradiate liquid plasma when RBCs for trauma patients aren't irradiated?
Emelie reacted to a post in a topic:
Why irradiate liquid plasma when RBCs for trauma patients aren't irradiated?
-
What brand of cell panels do you use for antibody identification (0,8-1%)?
Yes, we use BioRad gelcards and I know of their panel, looking for others as well, trying to "get to know the market". It might not be as large as I'd hoped though Hope to avoid cassettes (ie biovue) Thanks!
-
What brand of cell panels do you use for antibody identification (0,8-1%)?
Thanks! Forgot BioRad in my list, they do have a panel that's compatible with gel card technique, we've used it before.
-
 Emelie reacted to a post in a topic:
What brand of cell panels do you use for antibody identification (0,8-1%)?
Emelie reacted to a post in a topic:
What brand of cell panels do you use for antibody identification (0,8-1%)?
-
What brand of cell panels do you use for antibody identification (0,8-1%)?
Hi! The new IVDR regulation means all of our reagents need to be CE certified by may 2025. This causes us great trouble since a lot of our reagents and test cells are either prepared in-house, or acquired from nearest reference lab (who, in turn, produce them theirselves without CE certification). So, I probably need to find new test cells for antibody identification pretty soon. What producers are there? I know of Labex, Ortho, XboX lab, Nordic Biolabs and Tulip (indian). We'd like to continue using gel cards, so the panel needs to be 0,8-1%. Please help!
-
-
-
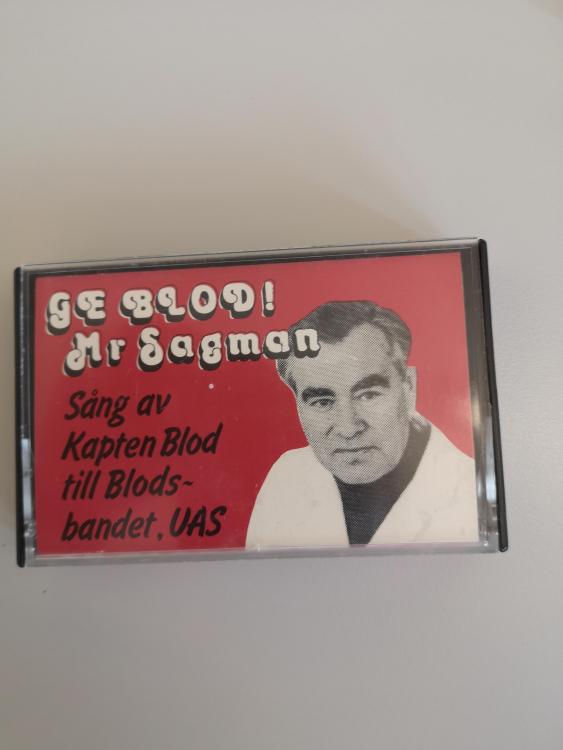
Oldschool
Found this old gem while cleaning out our retired doctor´s office. It´s Claes Högman, a real giant in Swedish blood banking, who (among other things) was a delegate in AABB during the 60's and recieved the Karl Landsteiner award, James Blundell award and the ISBT award. He sang in the Uppsala band "Blodsbandet" (transl Blood relations) under the name "Captain Blood". The song on the tape is "Give blood! Mr Sagman", which I suspect is a cover of "Mr Sandman"... Enough written, now I've gotta go find a cassette player!
-
-
-
Patients with blood type A Bel, what to transfuse?
It's Martin who's analyzed it (we've sent new samples so they can confirm their findings) We'd better do as they say, then 😄
-
-
-
Patients with blood type A Bel, what to transfuse?
Thank you! I found it difficult to find general recommendations regarding Bel. I discussed it with our reference lab just now, they weren't convinced about the transferase's ability to produce a complete antigen, since the expression was extremely low. I thought, as you say, that the absence of anti-B would implicate a normal B antigen but they were unwilling to recommend anything but A or 0 blood. This particular patient has a mutation not earlier documented, so it might be their cause for taking extra caution. Thank you for some great insight! It's an amazing forum for gaining new knowledge!
-
Patients with blood type A Bel, what to transfuse?
Hi! We have a patient who genotyped as A Bel. Is the Bel subgroup a complete antigen or partial? The patient expresses extremely low levels of B, would it be safe to transfuse with AB blood? The patient has no detectable anti-B occurring naturally. As far as I can tell by the litterature, Bel cells are not agglutinated with anti-B (but do bind to them)? We will, of course, have our doctor decide what recommendations to give, but I would like to know how other treat these patients as it´s a first for us. Please explain it like I´m five :)
-
BloodBankTalk: Antibody/Antigen Reaction
I just answered this question. My Score FAIL
-
-
 Malcolm Needs reacted to a post in a topic:
BloodBankTalk: Clinical Aspects of Transfusion Reactions
Malcolm Needs reacted to a post in a topic:
BloodBankTalk: Clinical Aspects of Transfusion Reactions
-
BloodBankTalk: Clinical Aspects of Transfusion Reactions
I just answered this question. My Score PASS
-
BloodBankTalk: Antibody/Antigen Reaction
I just answered this question. My Score PASS
-
BloodBankTalk: Correct Blood Bank Nomenclature
I just answered this question. My Score FAIL
-
 Malcolm Needs reacted to a post in a topic:
BloodBankTalk: Blood Transfusion Therapy in Haemoglobinopathies
Malcolm Needs reacted to a post in a topic:
BloodBankTalk: Blood Transfusion Therapy in Haemoglobinopathies
-
BloodBankTalk: Blood Transfusion Therapy in Haemoglobinopathies
I just answered this question. My Score PASS
-
BloodBankTalk: Antibody/Antigen Reaction
I just answered this question. My Score FAIL
-
-
BloodBankTalk: Antibody/Antigen Reaction
I just answered this question. My Score PASS