Everything posted by Emelie
-
General Lab: Dilution
I just answered this question. My Score PASS
-
What brand of cell panels do you use for antibody identification (0,8-1%)?
Yes, we use BioRad gelcards and I know of their panel, looking for others as well, trying to "get to know the market". It might not be as large as I'd hoped though Hope to avoid cassettes (ie biovue) Thanks!
-
What brand of cell panels do you use for antibody identification (0,8-1%)?
Thanks! Forgot BioRad in my list, they do have a panel that's compatible with gel card technique, we've used it before.
-
What brand of cell panels do you use for antibody identification (0,8-1%)?
Hi! The new IVDR regulation means all of our reagents need to be CE certified by may 2025. This causes us great trouble since a lot of our reagents and test cells are either prepared in-house, or acquired from nearest reference lab (who, in turn, produce them theirselves without CE certification). So, I probably need to find new test cells for antibody identification pretty soon. What producers are there? I know of Labex, Ortho, XboX lab, Nordic Biolabs and Tulip (indian). We'd like to continue using gel cards, so the panel needs to be 0,8-1%. Please help!
-
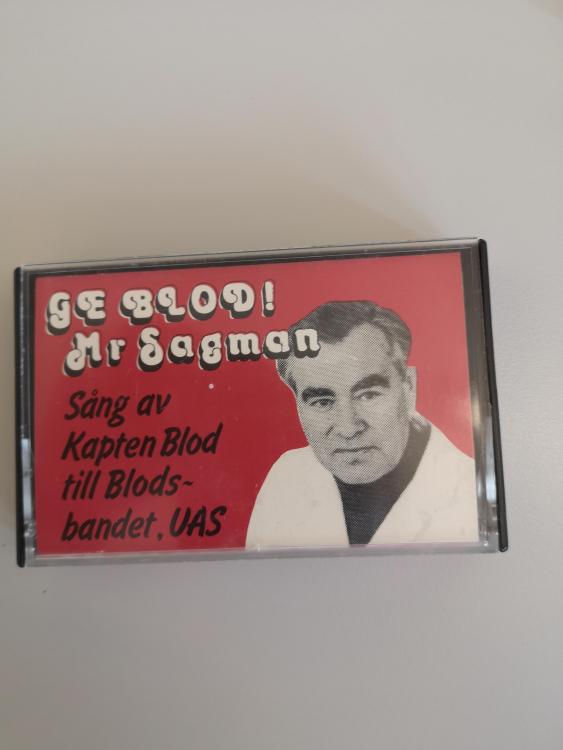
Oldschool
Found this old gem while cleaning out our retired doctor´s office. It´s Claes Högman, a real giant in Swedish blood banking, who (among other things) was a delegate in AABB during the 60's and recieved the Karl Landsteiner award, James Blundell award and the ISBT award. He sang in the Uppsala band "Blodsbandet" (transl Blood relations) under the name "Captain Blood". The song on the tape is "Give blood! Mr Sagman", which I suspect is a cover of "Mr Sandman"... Enough written, now I've gotta go find a cassette player!
-
Patients with blood type A Bel, what to transfuse?
It's Martin who's analyzed it (we've sent new samples so they can confirm their findings) We'd better do as they say, then 😄
-
Patients with blood type A Bel, what to transfuse?
Thank you! I found it difficult to find general recommendations regarding Bel. I discussed it with our reference lab just now, they weren't convinced about the transferase's ability to produce a complete antigen, since the expression was extremely low. I thought, as you say, that the absence of anti-B would implicate a normal B antigen but they were unwilling to recommend anything but A or 0 blood. This particular patient has a mutation not earlier documented, so it might be their cause for taking extra caution. Thank you for some great insight! It's an amazing forum for gaining new knowledge!
-
Patients with blood type A Bel, what to transfuse?
Hi! We have a patient who genotyped as A Bel. Is the Bel subgroup a complete antigen or partial? The patient expresses extremely low levels of B, would it be safe to transfuse with AB blood? The patient has no detectable anti-B occurring naturally. As far as I can tell by the litterature, Bel cells are not agglutinated with anti-B (but do bind to them)? We will, of course, have our doctor decide what recommendations to give, but I would like to know how other treat these patients as it´s a first for us. Please explain it like I´m five :)
-
BloodBankTalk: Antibody/Antigen Reaction
I just answered this question. My Score FAIL
-
BloodBankTalk: Clinical Aspects of Transfusion Reactions
I just answered this question. My Score PASS
-
BloodBankTalk: Antibody/Antigen Reaction
I just answered this question. My Score PASS
-
BloodBankTalk: Correct Blood Bank Nomenclature
I just answered this question. My Score FAIL
-
BloodBankTalk: Blood Transfusion Therapy in Haemoglobinopathies
I just answered this question. My Score PASS
-
BloodBankTalk: Antibody/Antigen Reaction
I just answered this question. My Score FAIL
-
BloodBankTalk: Antibody/Antigen Reaction
I just answered this question. My Score PASS
-
Irradiating blood products for mod size hospital
Tricore; yes, in Sweden many larger hospitals use PI instead of irradiation when preparing platelets, the methods are equivalent. In moderately sized hospitals it's more convenient and cost efficient to irradiate the (rather few) components needed at the irradiation center instead.
-
Irradiating blood products for mod size hospital
We are our own blood suppliers and we too cooperate with our hospital's irradiation center to irradiate blood products. If they weren't able to accomodate our demand we might switch to pathogen inactivation, such as Intercept, for the platelets and hope the irradiation center are willing to handle the smaller amount of RBC's.
-
transfusion reactions
The physician rates the reaction from mild to severe where I work, if the reaction is considered mild, we don't do anything other than document it in the computer system so that we can see if there are additional transfusion reactions connected to that specific blood donor, or if a certain patient often has a reaction. If we get a call about a suspected reaction and they don't send us any samples I usually just assume it was rated as mild, depending on what information I've gotten. We do not document the time ourselves, the nurses are required to fill in a form which covers all that.
-
New BB tech - need some comforting words
Where I work we're alone during nights and weekends, so situations that would have been perfectly fine daytime with a couple colleagues around can easily get quite overwhelming with only a doctor on call-duty to discuss with. Like when there's a traffic accident or some other trauma with several badly injured victims and one of them turn out to have a pos ab screen - it can be quite stressful to set up an ab panel while simultaneously handing out lots of blood and keeping up with the thawing of FFP, and if our stocks are getting low, managing the transfer of blood and platelets from other hospitals to our own. I rarely encounter those extreme situations, but I had a slightly annoying weekend a couple months ago, working alone, when an ER patient needed a lot of blood acutely and of course she had a pos ab screen with several ab's. There wasn't a chance for me to identify them properly so I phenotyped her thoroughly and cross-matched units. I tested her against more than 20 units that fit her phenotype as far as I knew (Rh, K, Fy, Jk, MNS) and still only found 2 that were compatible. She received a lot more units of rbc's that weekend and we do all xm manually, but the most frustrating thing was when our primary "help-lab" sent back the results from her blood work marked as "Un-identified antibodies"... and it's not a one-time only patient, this one was at the hospital for quite some time getting several more transfusions and will most likely be back. We've sent new samples to a ref lab and hope for more exciting answers this time In my opinion, it's important to always double-check with the medically responsible doctor before doing anything when you're uncertain, rather ask for expert advice one time extra than one too little, and document everything they say in order to keep your back free. As a blood lab tech I am not qualified to make decisions regarding patients, no matter what opinions I harbour (though it's obviously important to always give sufficient info about ab's and other findings to the patient's doctor to help them make proper decisions). And, of course, always do a background check on a patient when something seems really odd, bm transplants and recent transfusions at other hospitals can mess things up, and there might be important information to be had
-
RhD incompatible PLT transfusions
We only use apheresis plts, AB0 compatible for frequent recipients such as haematology pts since the cell survival is somewhat better, but do not consider Rh at all, unless we have had to buy pooled units from another supplier. We have strict limits reg the levels of rbc's in our apheresis products so it's only the plt ag we consider - i.e. no concerns regarding K either.
-
A curious case of anti-e
Galvania - No he did not react in the reverse grouping, we first encountered the patient when we were typing him a couple decades ago but there's not much historical information other than that the lack of anti-B was caused by his inability to create IgM. Unfortunately the patient passed away today, otherwise it might have been motivated to send samples to another, more sophisticated laboratory for eluating etc earlier on. I suspect his doctors knew he wouldn't last long anyway so they probably weren't very interested in our findings.
-
A curious case of anti-e
I washed the cells in order to aquire a neg result in the ctl well when performing the DAT I am trying to phenotype Rh+K but now after 2 washes the only thing that's changed is that all the reactions (including ctl) are even stronger and clearer... just out of curiosity, how many times is it reasonable to wash the sample before giving up? It's alright to wonder! I do not know how Blood transfusion departments perform the cold agglutinin tests, but at our microbiology dept, they titrate the patient's serum with NaCl and 0- blood and cold incubate over night. Titers > 1/16 counts as positive. The test is only performed to identify immunological/haematological disorders, and is not used to diagnose mycoplasma, the use PCR and PAAA for that.
-
A curious case of anti-e
Wow, thanks for the quick reply! I will certainly have another go at the Rh phenotyping if there is any sample left. I did however wash the rbc's in warm PBS doing the monospecific DAT and it didn't reduce the reactions, but I'll keep my fingers crossed (and wash more times)! Unfortunately, the cold agglutinin test is performed at the microbiology lab at our hospital but I'll see if there's anything I can do!
-
A curious case of anti-e
Hi Malcolm, and thanks for your answer! As we werent able to phenotype the patient due to his strongly positive DAT (I tried an Rh+K card but ctl turned out a strong 3+ just as everything else), we don't know wether or not he might have a real anti-e rbc ab, but we assume it is an autoantibody or, rather, a mimicking ab due to the strange reaction pattern and that the patient has no record of earlier transfusions. The haematologist treating him was certain it was cold ab's, but the cold agglutinin test from the laboratory came back negative. Still, we had those findings in our cold ab panel and the patient's rbc's turned into a solid lump as the blood cooled. New samples that were prepared and analyzed in 37°C didn't react differently than the earlier though, and cross-matching e- blood didn't turn out any better than e+. We will try to give the patient e- blood as far as possible, but we don't have that much to choose from in our bloodbank so he will probably receive e+ units further on too since we don't think it is a "true" rbc ab. It is very interesting to hear what those more experienced and who work with much more sofisticated methods has to say, I learn something new everyday!
-
A curious case of anti-e
A patient came to the ICU with Hb at 52. It was quickly concluded that he had some sort of hemolytic anemia. He also had an immunodeficiency since birth with low levels of both IgG and IgA, and was wholly uncapable of producing IgM. The doctor requested a monospecific DAT and a screen, and ordered 2 bags of blood. All my lab tests came out as 3+ straight over, including the ctl well, so I proceeded with an antibody identification. Unsurprisingly, the patient's plasma gave 3+ reactions against all panel cells as well as his own rbc's, both with IAT/LISS (gel) and PEG. Autoadsorption x2 gave no other outcome, not even the slightest reduction of reactions. I cross-matched blood (again, 3+ reactions) which the patient received without any reported transfusion reactions. When I had the results from the cold ab panel on NaCl gel cards it clearly showed an anti-e at all temperatures (4, 20 and 37°C). Since the panel is used to identify IgM antibodies I assume that this is an autoantibody of IgM-type, and not a regular IgG anti-e, possibly caused by the IVIg the patient has received? I have no clue. The hospital where I work isn't very large and we don't do any advanced ab identifications ourselves, neither do we encounter these kinds of results and patients regularly. Is there anybody who has some ideas and would like to enlighten me? Would you have done any further investigation regarding ab detection?