Posts posted by SbbPerson
-
-
-
-
-
-
-
-
-
-
-
-
Edited by SbbPerson
spellingOn 3/7/2024 at 8:38 AM, Pamo said:How does one develop Antibody ID samples for training purposes?
Our blood bank do not do titers. We send those out to a reference lab. We only do screens and AB ID's. Usually, we use our Anti-sera for training, for screens and ID's. We also have a few patients with very interesting samples(multiple Allos, Weak D, DARA, Anti-Ku, etc...), we save those and use them for training too.
-
21 hours ago, Ward_X said:
My old lab used to do something similar! Just a dummy slide with the probe wedged in the well and putty sealing around the opening.
For those wondering if a thermometer will fit -- there are some that do, and the wiring threads out under the cover using a small notch

Wow. Nice. I think if Ortho required people to have one of those, it would have been supplied with the workstation, instead of people just rigging something up.
-
Edited by SbbPerson
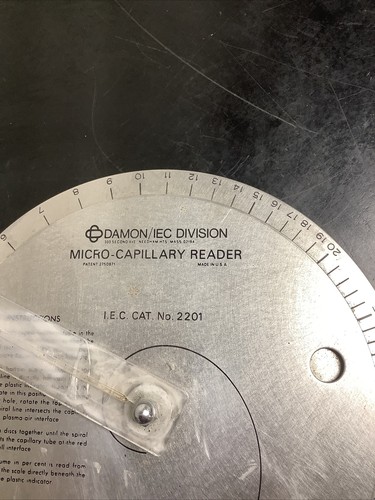
On 2/26/2024 at 12:47 PM, Ward_X said:My lab has been dealing with a broken micro-capillary reader for too long, and I've been looking at trying to find a replacement/alternative that isn't found on eBay.
We currently have the beloved wheel and centrifuge combo by Damon/IEC Division, but they unfortunately stopped manufacturing these.
What does your lab currently use?
We stopped using a crit reader. We now have a hemoglobin reader. It's electronic. Ours is the Hemocue 201 model.
-
Edited by SbbPerson
20 hours ago, Kim D said:How are you documenting temperature of headblock in new combo system?
green light ?
We do the same as Ren_Hh , we put a check mark on the daily temperature log. The tech support people assured us that the green light means the system is within acceptable temperature(approx. 36 to 38 C) range. Besides, good luck trying to find a thermometer small enough to fit into those heating blocks/wells with the cover closed too.
-
On 10/5/2023 at 2:27 PM, Mabel Adams said:
Does anyone know of a program for training EMTs and Paramedics how to store and transport blood products as well as transfuse safely (which will probably be a rare task for any one individual)? And then how about a process to assess that they are remaining competent? I don't want to administer such a program as I already have a full-time job but would like to point them in the right direction or make clear what it would take to accomplish this. We might consider providing liquid plasma if they can check all of the required boxes. Our Air Ambulances already carry blood products, but they get a lot of opportunity to transfuse and are accustomed to following strict FAA regulations. I think a lot of them are RNs also. This would be ground ambulances.
I think the EMTs for our helicopter service does transfusions. We just switch out their LTWB O Positive units every 30 days or so. The units hardly ever get used. I will try to find out more information if I can.
-
On 2/7/2024 at 2:20 PM, JT Super said:
Hi, I was wondering where in the AABB technical manual states the timeline of repeating the antibody panel for a historical patient? Is it 2 weeks, 3 weeks, or every 3 days? Which is the most common and safest practice?
5.14.4A new sample shall be obtained from the patient within 3 days prior to transfusion in the following situations:
- If the patient has been transfused in the preceding 3 months with blood or a blood component containing allogeneic red cells.
- If the patient has been pregnant within the preceding 3 months.
- If the history is uncertain or unavailable. Day 0 is the day of draw.
5.14.5In patients with a history of previously identified antibodies, testing shall be capable of detecting and identifying the presence of newly formed clinically significant antibodies. Standard 5.14.3.1 applies.
5.14.3.1When antibodies are detected, additional testing shall be performed to identify antibodies of clinical significance.
Source: AABB Standards for Blood Banks and Transfusion Services, 33rd Edition, effective April 1, 2022 (Published: 12/21/2023 )
-
On 1/6/2024 at 7:41 AM, Cliff said:
That's odd.
I was under the impression (possibly false) that PayPal was only required for me.
Anyhow, I just added Stripe payment processing. When you get to the checkout, you can choose Stripe or PayPal.
I appreciate your support!
Thank you Cliff! Sorry, I didn't see this reply sooner. Thanks again
-
On 11/9/2023 at 7:51 AM, Jimmy Lowery II said:
Hello! I’m a long-time blood banker who has recently entered the world of microbiology. This forum has been such a great resource during my time in transfusion, so I’m hoping that the microbiology folks could answer a few questions related to WBC smears. I am interested in learning more about the workflow for this test and how these are prepared and read in different facilities.
In your facility, are these typically done in microbiology or hematology?
What stain are you using for WBC smears in your lab?
We use the same stain we use for hematology slides, wright-geimsa. If we see WBCs, the result is a qualitative "present" or "none seen". Usually, if there is an infection, it will be mostly neutrophils.
-
-
To whom this may concern,
Last year, Paypal canceled my account for some reason. I called them but they gave me a vague explanation. So my premium membership wasn't renewed.
Is there another form of payment we can use? Like a credit card or something. Thank you.
-
-
-
-




HemeLabTalk: Neutropenia
in Question of the Day