KBBB
Members - Bounced EmailContent Type
Store
Profiles
Forums
Blogs
Events
Frequently Asked Questions
Gallery
Downloads
Glossary
Links Directory
Questions
Jobs
Vendors
Everything posted by KBBB
-
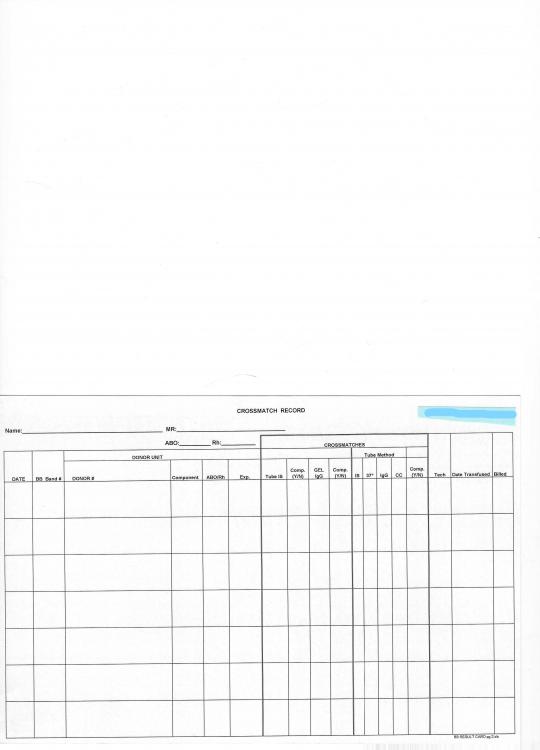
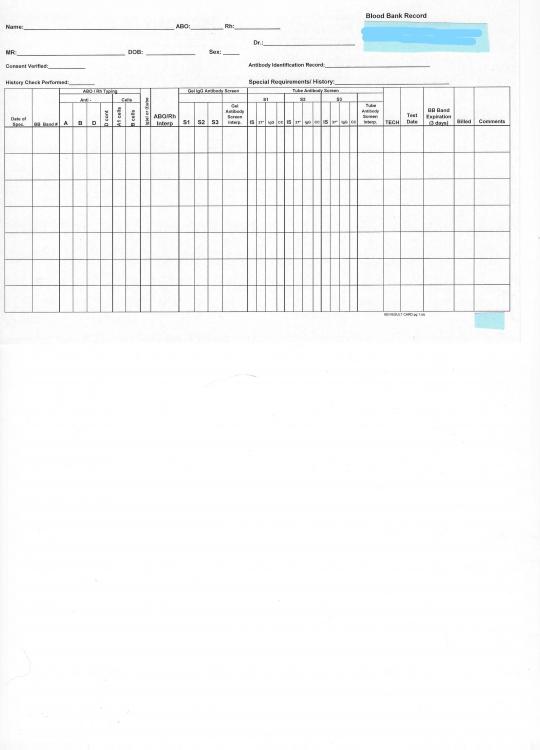
Here's an example of a front and back card used in a Transfusion Service without a computer system. (Was all manual but relatively small operation). The cards were closer to 6x8. Designed using Excel, then printed onto 8 1/2 x 11 cardstock with standard lab printer (front, then back, then cut in half & trimmed to fit the box. (Low budget). I can email to you directly if the scans don't come out very well. All results were written directly on the cards with all crossmatch and transfusion info on the back. Lab subsequently closed and transfusion service went back to central blood center.
-
Darkening of panel cells-possible contamination?
KBBB replied to KBBB's topic in Immunohematology Reference Laboratories
The supplier of the panels and the storage solution is the same. Supplier says no one else is having a problem. If we have 2 sets of the same lot of panel, we have seen vials in one set go dark while the same vials in the other set is fine. -
We use multiple suppliers of panel cells as well as make an in-house panel from frozen donor cells. Over the last year we have noticed several vials in multiple lots of commercial panel cells from one supplier going dark (contaminated?) as well as our in-house panel cells that are suspended in commercial red cell storage solution. Has anyone else noticed this type of problem with any of your commercial panels? Have you ever had the problem and figured out what was causing it? We have considered fungus or bacteria getting into the vials, but can't really explain what is going on with the two different issues. We are looking at another brand of modified Alsever's solution to try for our in-house panel but that doesn't solve the commercial panel mystery. Any thoughts?
-
We had another one of these issues today. 0.8% Surgiscreen Lot VSS439 Cell #3 Donor 309401. Reacted 2+. The Antibody ID sent to a Ref. Lab was negative. An Antibody screen using 3% set (Lot 3SS478) diluted to 0.8% for gel testing was negative.
-
One more thing to remember and has been discussed before in this forum-- any labels stuck to blood components have to be FDA compliant with regards to the adhesive used. Avery labels are not approved for affixing to blood component bags. Shamrock is one label Co. that I know that has blood bank labels that have approved adhesive (it is stated as such in their catalog). There are probably others.
-
What is the donor number? Ortho may use the same donor for different lots of screening cells. We had an issue with VSS432 Cell #1 donor 308439 with a weak reaction. We sometimes resolve questionable results by diluting the 3% screening cell set to 0.8% for gel. If that is negative, we interpret as negative. It seems to me that if it was a storage issue, then multiple patient plasmas would show the same problematic reactions. We also have had the experience of sending a specimen to the reference lab for a 1-cell reaction, only to be told it's a cold autoantibody. It doesn't make sense to me that the cold auto would only react with 1 cell and not all three. The cold is there, but it isn't the explanation for the reaction. We also have had sample reactions that are explained by rouleaux, but it isn't always very obvious.
-
Cold Agglutinins in surgical patients for CABG
KBBB replied to Ardele Hanson's topic in Transfusion Services
The OR suites at the hospital I used to work at were much colder than usual Rm Temp. We had to do a 4 deg. and 22 deg. 15-20 min incub. screen...2 drop patient plasma, 1 drop patient cells. If the result was 2+ or greater (if I remember right), we had to call the OR. We just wrote them on a log since we couldn't figure out how to do this in the computer system without causing issues. This mandate was from the head (and big Kahuna) of Cardiac Surgery. We also had a reference in our file from the Dr. and he had some personal bad experience. -
Has anyone had to deal with a Tech who doesn't label tubes for unit re-typing? ...or does anyone not require it because it's "only unit re-typing?" I am an indoctrinated Blood Banker and label everything.
-
We need to think about which class of antibodies are being tested. When doing a gel or tube AHG crossmatch using anti-IgG we are looking for reactions between the antigen and an IgG antibody. When doing the IS crossmatch at Rm Temp, the phase favors the reaction between the antigen and an IgM antibody. The percentage of IgM vs IgG and the titer of anti-A, anti-B, and anti-A,B varies from sample to sample. We generally think of ABO antibodies as IgM, but they may be a variable mixture of IgM, IgG, & IgA. So only doing an AHG crossmatch, or prewarming, which decreases the possibility of IgM antibodies reacting, will not always detect an ABO incompatibility especially if the sample only contains IgM ABO antibodies. This is also why I don't think "validating" a system to detect ABO incompatibility makes sense since the samples are so variable. Thus the conundrum! It seems the only way to avoid doing the required IS crossmatch to detect ABO incompatibility is to take away any possibility of an ABO incompatibility in the first place...Use group O.
-
In the case when the Gel IgG crossmatch is compatible (performed because the patient has clinically significant antibodies), but the IS crossmatch is incompatible due to clinically INsignificant antibodies, there have been a couple of suggestions. I would like to know what the CMS answer is, but haven't seen anything about this to date. One person suggested that the IS testing could be prewarmed but another Tech asked whether the prewarmed Immediate Spin procedure detected ABO incompatibility. (no answer given) Since IgM antibodies react best at RT or below, warming the system will decrease the reactivity of the ABO IgM antibodies. That's why I don't think prewarming is a valid answer. Another suggestion is to use group O RBC's. It seems that this would be a valid answer because the concern for ABO incompatibility no longer would be an issue. Just using logic here. Here in the US, if we order Ag-typed units for a patient with antibodies, the blood supplier will usually have group O available because it is more efficient/cost effective to Ag type O donors for this reason. (I currently work in a small lab that sends all antibody ID's to the Ref. Lab and we don't keep antisera on hand for Ag typing. We also do not have a computer system...all manual.) Just to clarify for international members, in the US we are required to retype all units that are procured from the blood supplier. ABO on all units, and also IS D on all Rh neg. units. The Gel IS XM (which I have never actually done) would detect IgM ABO antibodies because there is no incubation time at 37C. The cells and plasma are added to the buffer card and centrifuged immediately...you will get your result...in 10 minutes...which is why we use the tube method. And finally, just a little information on Electronic "crossmatch" (even though the last lab I worked at didn't have it set up, I investigated the requirements for the computer). The computer algorithm decides whether the patient qualifies based on the requirements set up like...the patient has no historical or current antibodies, ABO/Rh type has been done twice on same or different specimens...& there may be more. Basically, you just aren't doing the actual plasma/RBC crossmatch which saves a lot of time since almost all of the time, the IS XM is negtive. Your crossmatch tags won't print out unless everything is ok. I think that maybe because the 1st rule to use the electronic crossmatch requires the antibody screen to be neg. and historically neg., this is the problem that hasn't been clarified yet.
-
We will begin sending units to two other hospitals soon. Our plan is to tag the cooler with the patient last name only to comply with HIPPA. Also, blood for transfusion is not considered a Biohazard. I think I found that info in the Technical Manual somewhere.
-
We have ThermoSafe Transporters for sending blood to outlying hospitals. If you have these, do you "lock" them in any way? We don't want to break the zippers, which I'm pretty sure will happen if a plastic lock is strung through the holes in the zipper pulls. I can't find that there is any requirement to do this. We will use couriers and there is a concern by one person that the containers should have some sort of tamper proof system so the couriers don't "mess with the blood". Any suggestions?
-
Is this the standard out there? I don't have the Ortho procedure in front of me, but do they say to call a patient 'Rh D negative' if the reaction is less than a 3+ reaction on their ABD cards? Do others call any reaction for gel D, ' Rh D positive'? ...or do you then do a tube Rh and use the tube result for your interpretation (wk D not required for recipient testing)? If the D typing in gel is more sensitive, but for those few patients who are wk D we ignore the more sensitive aspect and revert to the less sensitive tube test, do we use the logic that it only affects a small number of patients? We have to use the gel cards (reagent contract), and will also have tube testing available for unit retypes and backup patient testing. Our transfusion service will only be serving an adult population.
-
Blood Unit Returns After Issue-Please refresh my memory
KBBB replied to Brenda K Hutson's topic in Transfusion Services
It seems that if we all use more descriptive titles for the threads, we might be able to find them again in the future. As I recently started watching this site more and more, it has become apparent that when the title isn't specific it makes it really hard to pick the subjects we would like to view that are applicable to our situation. Is there a way to re-title the thread that is more specific? One transfusion service I know has set their HCLL computer system to allow return of units if within 30 min of issue. That was probably based on the policy set in the past based on something common at the time. It is unfortunate that it seems so difficult to find out what we are really supposed to be doing until some inspector cites the lab. The CAP requires certain things, Joint Commission isn't as specific... not all are inspected by FDA, but we want to follow those rules too...and here we find out about other countries. Is it any wonder that different labs have so many different requirements and processes? No wonder we get stressed out!! -
Everyone...please re-read post #1 and #4. This IS NOT a hiring issue but the posters have morphed it that way. There are a lot of "ifs" and "assumptions" being made. Admonishments and points taken...
-
The source is reliable. More than one source reported poor performance but I would rather not go into the specifics. People generally do not offer the information that they were terminated from their last job, or allowed to resign rather than be terminated. That is why opinions of other Med Techs who previously worked with a prospective candidate can be invaluable. If they somehow have info to share (liked they actually worked with them at another hospital), then it is fair game. Hiring is ultimately up to the Director and they can ignore any and all information. They will find out for themselves soon enough. All your comments are good points to consider. Thanks for the input.
-
Thanks Marilyn! You bring up several great points that I will remember as the issue continues. I found out about the situation by speaking to a former co-worker of this person (not a supervisor). The person in question stated that they worked in BB at that hospital, but didn't offer up any other info. There was no on-site transfusion service when the person was hired. My first impression and from examples from others is that there is a lack of focus/ attention deficit (ADD??) (I'm trying to keep this a little vague). From what I understand about the error, it should have been reported to the FDA.
-
Thanks for the input. There is no BB computer, so no computer crossmatches and no automation. As to the expense, I haven't done the cost analysis yet, but time is money too. No cord bloods (not that kind of hospital). Antigen typing isn't an issue yet since we are just starting up the transfusion service and won't be doing panels in the beginning. I just barely started working there and working on this project (week #2) We can get Ag typed units from the blood center. We also won't be doing DAT's at first (other than maybe for any transfusion reactions...figuring that all out). I suspect the number of DAT's ordered is low.
-
If you knew that a Tech in your lab previously worked at another hospital and made an ABO typing error that resulted in dismissal, would you try to train that person to work in your transfusion service? ...and BTW...without a BB computer system. (Assume that they have adequate certification for the state/facility)
-
Hi, I have worked in several other hospitals that did MTS gel Antibody Screens and panels, but did ABO/Rh testing by tube. It was because the tube testing is cheaper (and of course faster). We only have one MTS centrifuge. What are your opinions on the comparisons of the gel and tube methods for ABO/Rh testing on patients and retypes on units?
-
Hi, The hospital I work for has rec'd the MTS Gel equipment for starting an in-house transfusion service. Included is the MTS electronic pipette. I previously used the 3-vol. repeating pipette at other hospitals. I am told that they don't make the manual adjustable 3-vol ones anymore. I'm finding the electronic one a little cumbersome to use (that is the tactful version). I would like to hear what others think about it. Thanks PS: If this has been discussed before, please direct me to the post. I couldn't find anything, at least not quickly.
-
I'm going with BloodBanks' reply-thanks. Even though there are other opinions, based on my experience with inspections and this issue at other facilities I don't think it is considered valid to assume complement is coating the cells without directly testing for it. I don't want to get into producing complement check cells either. Different inspectors have different opinions based on their training and expertise. The only way to stop the gray areas is to write the questions plain and simple. example...."If your lab is performing DAT's and reporting results for Complement-coated cells, you must use anti-C3b, C3d and verify the reagent performance by the use of complement-coated check cells" I'm sure you all have seen labs "get away" with something because the inspector didn't notice. You may think you have a valid argument until an expert at the CAP/Joint Commission corrects you. That's why inspections can be so stressful!!!!
-
I searched in the previous threads and didn't find an answer to this either. There were only 2 ordered DAT's at our facility in the last year, and just a few transfusion reaction workups. We could: 1. Send all DAT's out to the local ref. lab. (thus getting rid of Poly AHG and anti-C3d,C3b (this facility had not previously had the C3d,C3b check cells....which is deficient, and none of the previous inspectors noticed-JCAHO-inspected). 2. Keep Poly AHG and do a DAT screen...sending out any positives to the ref. lab. Is it considered incomplete on the CAP survey to do some but not all types of DAT's? Note that our facility does not have an OB service. I'm interested in what others have done in this situation and your opinions. Thanks