Everything posted by AMcCord
-
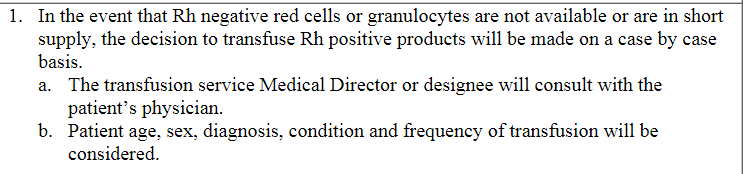
Transfusing O positive RBCLR to O negative
Below is our policy for switching Rh negative patients to Rh positive red cells for non-emergent cases. We would document that decision and any pathologist instructions in the patient's profile. For emergency release/MTP we follow policy and do not notify the provider unless it is a patient under 19 years or a female of child bearing potential.
-
FDA exceptions to 21CFR640 and receiving products from suppliers
Good info - may have to update our SOP.
-
FDA exceptions to 21CFR640 and receiving products from suppliers
Have you contacted someone in Omaha or St Paul in their quality section? Should be someone there with knowledge about that process.
-
Anti-CD36 (anti-GPIV) Frequently Interferes With Routine Red Blood Cell Antibody Testing in Patients of African Descent-References?
Thank you!
-
Anti-CD36 (anti-GPIV) Frequently Interferes With Routine Red Blood Cell Antibody Testing in Patients of African Descent-References?
I didn't find much either, but from what I did find it looks like it could be another interesting blood banker's problem since CD36 is definitely found on RBCs. And it sure looks like it may be utilized with immunotherapy for multiple kinds of cancer treatment to make it more effective. Or for FNAIT. https://pubmed.ncbi.nlm.nih.gov/1382721/ The link below is interesting - not sure how it would relate. https://pubmed.ncbi.nlm.nih.gov/8623134/ And then there are these tidbits: https://pubmed.ncbi.nlm.nih.gov/34041523/ https://www.ahajournals.org/doi/full/10.1161/01.atv.16.7.883 If patients with African descent are more likely to develop anti-CD36 due to CD36 deficiency, are their red cell ABO types (or other antigen types) going to be affected by that antibody (which would be an autoantibody)??? I'm with Mabel - anyone out there know anything about using anti-CD36 for cancer treatment or FNAIT treatment?
-
CAP ALL COMMON CHECKLIST COM.04250
I like it Mabel! We all need to start using that for our CAP inspections to see if we can shove them in the right direction.
-
Rh antigen typing on Vision
We are doing both. We use automation at this time only for cord blood specimens, but having a survey will save us from the alternative testing issue on the All Common CAP checklist.
-
Blood unit patient label
Ours print on a 4" x 4" label from a Zebra type printer. We stick them on a slightly larger tag made from card stock with an eyelet at the top for a rubber band. The back of the card stock tag is printed with a list of transfusion reaction symptoms and a brief description of response expected. Below that are blood handling instructions/education. All nursing documentation is in Epic.
-
Rh antigen typing on Vision
Bet they will sooner than later as more antigen typing is automated. I was delighted when the DAT survey for automation came out, even if it is ungraded for now.
-
CAP ALL COMMON CHECKLIST COM.04250
Exactly! We have to do it, but make the plan 'reasonable' for your facility.
-
Platelet swirl revisited
The ARC told us to put the chilly platelets in the incubator and let them rock for a couple of hours, then recheck for swirl. If they look good at that point and our pathologist is OK with that (which they usually are), we put them into inventory. We will use the unit(s), if we need to, until we restock. If the patient can wait for the next shipment, we hold off. Fortunately we only see this problem once or twice every winter.
-
CAP ALL COMMON CHECKLIST COM.04250
Job security??? My comment about several of the All Common checklist items is "we ain't chemistry!". Not that it gets me anywhere. Since we are in our inspection window, I made emergency changes to my SOP/form for that and we will scramble for suitable specimens. Our problem is finding enough suitable antibodies with sufficient sample volume to do all this extra testing. As part of our Patient Blood Management program we draw minimal patient specimens - just enough to do the ABS and an antibody ID if it isn't a warm auto workup. We can squeak extra antibody screens out if the patients Hgb is low enough, but not multiple ID panels. My only solution to that is to do abbreviated panels using 3 Ag positive cells and 3 Ag negative cells, then state that the results are consistent with the antibody IDed with solid phase. If that's not good enough - (bad words).
-
CAP ALL COMMON CHECKLIST COM.04250
We are in our inspection window now, so I'll let you know how we come out on that one.
-
Microscopes
If the model is discontinued and no parts are available for repairs, I'd say it has reached its 'end of life' - however I'll bet it will still work a long time after that before a part needs replaced (especially older, quality scopes). I can see 'end of life' for more complex or expensive equipment, but a microscope for blood bank is more of a minor equipment purchase. My 'new' scopes are student scopes that cost less than $500 and they work just fine for our purposes.
-
Dr Peter D Issitt.
Condolences to his family. Such a legend in our Blood Bank world.
-
Post-partum workup
Oh yeah! That was fun (sort of).....
-
Immune Hemolytic Anemias- Petz and Garratty
Thank you for sharing. Amazing career.
-
Patient hx
Especially slide 25 .
-
Patient hx
We don't issue cards to patients with antibodies. I've discussed it with several of our medical directors, but none of them have been very enthused. They feel that most of the cards will be lost, forgotten about, or the info won't get passed on to us. Based on our past experience, I can't make a strong case. Our current medical director is a believer in Med Alert bracelets for the scary stuff. I've seen only a few cards, under the following scenarios: A few times: nurse is checking out blood and says 'Oh, the patient showed me this card about an antibody or something. Did you need to see it?' YES, before you transfuse! Twice: nurse has started transfusion and calls Blood Bank - 'Mr XYZ showed me a card about an antibody or something today (or yesterday). Do you need to see it?' YES, STOP THE TRANSFUSION! and once, once only - as the patient was being admitted on the floor, the nurse called and said the patient had a card about transfusions - 'Do you want me to fax you a copy?' YES! Gold star for you! Sometimes I wish we could put a chip in the scruff of everybody's neck that had all that info loaded on it - allergies, antibodies, med history - wouldn't that be handy.
-
Post-partum workup
Nothing is ever simple, is it? Especially when you get other folks involved. I stopped a dose of RhoGAM from being given to the baby. I've had nurses squirt some out of the syringe because "it's an early miscarriage, they don't need the full dose". I asked how they were calculating that dose and how did they know how much they squirted out...no answer .
-
Post-partum workup
Oh yeah.... that dates us. And I remember doing antibody screens post RhoGAM, prior to patient discharge, to 'see if the RhoGAM dose was adequate'. No anti-D detected = give more RhoGAM. Something the OB folks thought seemed like a grand idea before the fetal bleed screen was available. Fortunately fetal screens came out about then. We were able to convince the docs to stop with the ABS orders by running parallel tests with the fetal bleed screen for several months to demonstrate how meaningless the antibody screen idea was..
-
Post-partum workup
If we've done an antibody screen when the patient was admitted, we cancel the screen on the RhIG workup. If the patient only had a blood type ordered on admission, we do a screen.
-
CAP Inspector Requesting Documents in Advance
That doesn't seem appropriate - check with CAP and see what they think. That said, it would sure make a one day Blood Bank/All Common inspection easier on the inspector to have the nitty gritty from SOPs checked off ahead of time. Those checklists are a BEAR timewise!
-
product modification labeling requirements...
With pictures???
-
product modification labeling requirements...
Would agree with that. Our software automatically 'thaws' and updates the unit outdate when we product select. Our potential failure point is that the tech who thaws and tags the product fails to change the outdate on the unit face label.