Malcolm Needs
Supporting Members ☆
-
Joined
-
Last visited
-
Country
United Kingdom
Everything posted by Malcolm Needs
-
HemeLabTalk: Malignancy
I just answered this question. My Score FAIL
-
Welcome bmhlabman
Welcome to this MARVELLOUS site bmhlabman. ENJOY!
-
Welcome Jigs
Welcome to this BRILLIANT site Jigs. ENJOY!
-
BloodBankTalk: Whole blood in massive hemorrhage
I just answered this question. My Score PASS
-
Welcome CisAB
Welcome to this Marvellous site CisAB. ENJOY!
-
Welcome Diane DT
Welcome to this FANTASTIC site Diane DT. ENJOY!
-
BloodBankTalk: Efficacy of granulocyte transfusion
I just answered this question. My Score PASS
-
BloodBankTalk: Massive transfusion protocols
I just answered this question. My Score PASS
- Welcome mhowell
-
anti-Jka likes to react unpredictably?
I should have also said that there is an excellent Blood Group Review available, viz Hamilton JR. An update to Kidd blood group system. Immunohematology 2024; 40: 28-33. DOI: 10.2478/immunohematology-2024-005.
-
anti-Jka likes to react unpredictably?
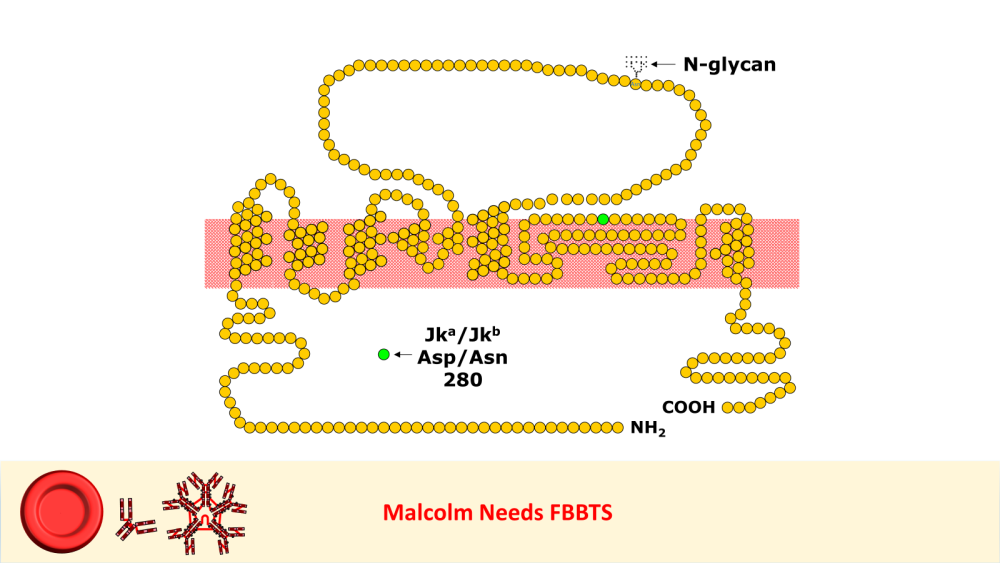
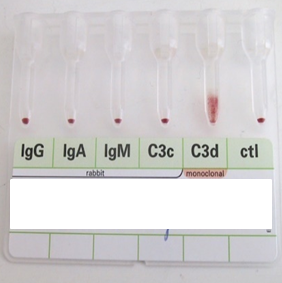
I worked in Red Cell Immunohaematology for most of my 43 years before retirement, including two times at the International Blood Group Reference Laboratory (IBGRL), and for over a decade at one of the NHS Blood and Transplant Centres in London. During that time, I saw some pretty weird Kidd antibodies, but never came across an example of one that reacted with red cells with Jk(a) heterozygous expression, but not with Jk(a) homozygous expression. One such "weird" type (although I never saw one) was the extremely rare, dominant inhibitor type In(Jk), similar, but, of course, not identical to In(Lu). These red cells usually type as Jk(a-b-), but their true Kidd type can be ascertained by Adsorption and elution tests.. These red cells are also more resistant to haemolysis by 2M Urea than red cells with "normal" expression of the Kidd antigens, but less resistant to haemolysis by 2M Urea than true "amorphic" Jk(a-b-) red cells. There are approximately 14, 000 copies of the Kidd carrier molecule per red cell (quite a small number, when compared with some other carrier molecules, such as the D antigen). The amino acid residue that defines either the Jka or Jkb antigens is very close to the red cell membrane in the 4th extracellular loop but is largely “hidden” by the 3rd extracellular loop (steric hindrance). Both facts may contribute to the weak reactions between Kidd antibodies and Kidd antigens. Schematic of the Kidd carrier molecule (after Wester ES, Storry JR, Olsson ML. Characterization of Jk(a+weak): a new blood group phenotype associated with an altered JK*01 allele. Transfusion 2011; 15: 380-392. DOI: 10.1111/j.1537-2995.2010.02795.x. In this paper, Wester et al also describe weakened forms of both the Jka and the Jkb antigens, but in each case, the amino acid substitution is remote from position 280 of the mature protein. In addition, an individual with the Trp171Arg mutation with weak Jk(a) expression has produced an anti-Jk3 or anti-Jk3-like antibody, and so they may be “dangerous patients” (Whorley T, Vage S, Kosanka J, Lose SR, Sandquist AR, Copeland TR, Westhoff CM. JK alleles associated with altered Kidd antigen expression. Transfusion 2009; 41 (Suppl.): 48A-49A (abstract). Lastly (for now anyway!), most foetal red cells sensitised by maternal antibodies react only with anti-IgG, but I (and a colleague Grant Webb) have both noticed, but not published, occasions when such red cells also react with anti-C3d and, in one case, only anti-C3d (see genuine photographs below)..
-
Welcome Jacquelyn
Welcome to this MARVELLOUS site Jacquelyn. ENJOY!
-
BloodBankTalk: Hemorrhage
I just answered this question. My Score PASS
-
Welcome ABanks
Welcome to this FANTASTIC site ABanks. ENJOY!!!!!!!
-
What's a high frequency antigen that might be weakened on expired reagent cells
You are quite right Jason. I also remember a similar paper, written by Jill Storry, entitled "Long term preservation of red cell antibody identification panels in low ionic strength solution." This was published in Medical Laboratory Sciences 1987; 44 (4): 350-355, but was based on the winning Margaret Kenwright award presentation at the Annual Scientific Meeting of the British Blood Transfusion Society, London, UK on 4th September 1986. This was when Jill was a Senior Medical Laboratory Scientific Officer at the South Western Regional Transfusion Centre of the National Blood Transfusion Service in Southmead Road, Bristol. She has done rather well for herself since then, now being a Professor at Lund University. Unfortunately, I don't have a DOI for this paper. At the time, I was working at Mayday Hospital in Croydon, London, and wrote to her to clear up a couple of queries I had. In early January 1988 she wrote back to me and, in this reply, she stated, "Can I also draw your attention to the fact that the original trial (her original trial) was done using frozen re-constituted red cells. It has subsequently been pointed out to me that when using fresh cells for screening purposes there is significant loss of Fy(a) and Fy(b) antigens over a two week period. This phenomenon has been well documented (see below) and is due to the release of proteases upon leucocyte aminoglycoside interaction. Gentamicin is of course, an aminoglycoside antibiotic. We have overcome this problem completely by leucocyte depletion using a Sepacell 500 filter, and I hope to submit a short communication to the IMLS journal describing the results of this modification." I haven't got a reference for this. The paper to which Jill was referring to in her letter was: Malyska H, Kleeman JE, Masouredis SP, Victoria EJ. Effects on Blood Group Antigens from Storage at Low Ionic Strength in the Presence of Neomycin. Vox Sanguinis 1983; 44 (6): 375-384. DOI: 10.1111/j.1423-0410.1983.tb03660.x All that having been said, I would be surprised if all screening cells and antibody identification cells were not now leukodepleted. In addition, of course, apart from certain areas of Asia, neither the Fy(a), nor the Fy(b) antigens can be regarded as high prevalence antigens, and those antigens within the Duffy Blood Group System that can be regarded as high prevalence (Fy3, Fy5 and Fy6) are vey different to both Fy(a) and Fy(b), and so it is doubtful that these would weaken substantially upon storage.
- Welcome Peter Paul
-
What's a high frequency antigen that might be weakened on expired reagent cells
True, but I was talking about the antigens on stored red cells, rather than the antibodies.
-
What's a high frequency antigen that might be weakened on expired reagent cells
Could be an antigen within the Knops Blood Group System. They are notorious for "going off" on older red cells, but the antibodies are not renowned for being clinically significant.
-
HemeLabTalk: White blood cells
I just answered this question. My Score FAIL
-
Welcome Triciasimm
Welcome to this fantastic site Triciasimm. ENJOY!
-
Welcome Craig Chalmers
Welcome to the truly awesome site Craig Chalmers. ENJOY!
-
Welcome AARONK
Welcome to this wonderful site AARONK. ENJOY!
-
Welcome Emma Williams
Welcome to this FANTASTIC site Emma Williams. ENJOY!
-
Welcome Littellallen
Welcome to this wonderful site Littellallen. ENJOY!
-
Letting tube sit to catch rouleaux or cold?
If there ARE extra reactions in the back type, then they do need to be resolved IF, and I mean IF, they look as if they could signify that the forward ABO type is false. That having been said, I STILL would not go looking for rouleaux or agglutination that was not present when the tests are read at their normal incubation period and temperature. Why would you want to look for a herd of Zebra, when you hear a herd of Horses (thank you John C Staley - or, at least, I think it was you who used to say this to me on a regular basis - apologies if it was not - but it was a great comment!)?