Content Type
Store
Profiles
Forums
Blogs
Events
Frequently Asked Questions
Gallery
Downloads
Glossary
Links Directory
Questions
Jobs
Vendors
Posts posted by BloodbankZ
-
-
I am looking into the billing for the CCP. We used 5 units under the EIND and I was able to find the attached file online. Has anyone else heard is there a HCPCS code yet? We are now in the Expanded Access Program and I know we will not be charged for those units. Does anyone know can you still charge for the thawing HCPCS#86927? TIA.
-
-
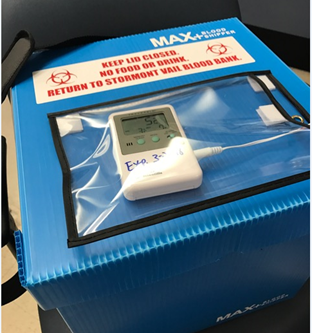
I have tried a data logger the Microlite III temp logger. It did not seem to instantaneously read the cooler temperature but just the temperature that the logger itself had been at. Conditioning it at room temperature it took several minutes before lowering in temperature when placed in a cooler with ice. I pre conditioned it in the refrigerator and it took a long time to read a higher temperature at room temperature. We store blood products in a cooler at bedside during surgery and need to account for the temperature. Do you have any brand suggestions?
-
I need to be able to monitor blood products while in a cooler such as at bedside in the OR during a surgical case. We currently use the BT10 indicators but I am needing a device to take a digital temperature reading of the cooler at intervals during the surgery.
Does anyone have any suggestions?
Thanks in Advance!
-
I was wanting to get input on DAT's performed for Transfusion Reaction Investigations. Do you perform them with just IgG, C3d or both? TIA.
-
Remote as in another location within the same hospital outside of the Blood Bank like the ER or OR.
-
I am looking at storing blood products in a remote location for our facility. Just curious what everyone is doing currently? Thanks for the info!
-
We use the Ortho Confidence System and AB plasma as our negative control. That will cover all of your possibility of reactions. Yes you would have to QC the ABD card as well. For Cord study we run the ABD w/Rev (in case the patient is AB POS you need the ctrl) and an IgG card well for the DAT. It may detect weak D but we perform a weak D test on every Rh negative newborn.
-
5 hours ago, AMcCord said:
You definitely want to check compliance with manufacturer's requirements whether you are using tube testing, gel, solid phase and/or automation. That said, validation is a must, though it doesn't haven't to be a huge project. Run split samples centrifuged using your current method, then using the new method. Tests should be representative - blood types, antibody screens as surrogate for indirect antiglobulin testing, direct antiglobulin testing, etc. - but don't have to be exhaustive.
We use Ortho gel primarily. It states nothing about centrifuge time. We use greiner tubes and they recommend 2000g for 10 min for platelet poor plasma. I am leaning towards the Stat spin express which is 3 minutes at 4000g. As long as it validates I don't see a problem do you?
-
Check EBAY I picked up a Clay Adams Serofuge there to "revitalize" one of ours. I think it was only $400.
-
23 minutes ago, BankerGirl said:
We use the Hettich and spin at 8000 rpm for 2 minutes. Works great but it does has a latch check that takes a about a second to complete, so if you are really fast at pressing the start button, it won't start immediatedly. I don't usually have a problem with it because I let it do it's thing, but occasionally I will be too fast and have to press start again.
BankerGirl do you know the g force?
-
I am looking to cut down our TAT. We currently spin our specimens for 10 minutes. Any suggestions for stat centrifuges? TIA.
-
I am needing some help setting up electronic crossmatch in Meditech. I have everything else in place but can not figure out how to prevent EXM in patients who have mixed field reactions. I am wanting to be able to perform the IS serologically as I understand this is needed per CAP and FDA regulations. Has anyone else experience this. We are currently on version 6.08. Thanks in advance!
-
On 3/10/2018 at 4:30 AM, gagpinks said:
If patient on DARA how soon they can develop pan-reactive antibody? We had our first patient who is on DARA had negative antibody screen before treatment after 36 hours of treatment antibody screen is positive in all 3 cell line. Patient's antibody panel shows some pan-reactive reaction with 8 out of 11 cells .But auto is negative . Is it due to DARA or patient is developing some allo antibody?
I would say it is due to the DARA. DTT treated cells will eliminate the DARA reactivity and let you be able to rule out everything besides mainly Kell system which DTT denatures. We perform a baseline type and screen and DNA HEA typings on patients before they start. If DTT screen is negative we give K negative cells if patient is antigen negative.
-
When I tried to run it in gel I never could get nice clean reactions. Their would always be particulate at the top of the wells. I have seen several tube procedures that are just using so many drops of 4% cell suspensions instead of concentrating their cells and then getting an exact 4:1 ratio with DTT. I have since went to doing it in tube. What kind of steps are you performing?
-
-
I was wondering if anyone knew of a report that showed incident rate of FDA reportable events per hospital or per other statistic like transfusions, patients, etc... Just looking for a baseline to see how our facility compares to others. I have searched and reached out to other facilities and haven't had any luck. Thanks in advance.
-
Has anybody tried DTT treating reagent red blood cells in MTS gel method? If so are you concentrating your cells before treating or have adjusted your ratio of DTT to the .8% suspension? TIA.
-
What are other people's institutions practices on the following. If you have a patient with an anti-D do you need to go ahead and carry out the D antigen typing on the patients rbcs through the IAT phase(weak D testing)? The AABB 18TH ed. Technical Manual states on pg. 327 "When the D type of a patient is determined, a weak D test is not necessary except to assess the red cells of an infant whose mother is at risk of D immunization." It then goes on to say under Identification of Antibodies to Red Cell Antigens pg.401 "Determining the phenotype of the autologous red cells is an important part of antibody identification." We use MTS gel for as our primary method for blood type determination and it states that Most weak D antigen expressions will be detected(which means not all), however partial DVI epitope variant of the D antigen will not be detected with this monoclonal reagent. Not that it really changes how we transfuse the patient but just curious to others procedures/thoughts. Thanks in advance.
-
Did you ever figure this out I am trying to get the same thing done with no luck.
-
We have been using Ortho Gel since 2008 we have serviced our Tipmaster pipettes several times. We are needing something new has anyone used the Vista Ovations for Ortho Gel or have another suggestion. Thanks.
-
Okay so I was always taught to use the rule of 3, 3 positive reactions and 3 negative reactions for peforming an antibody ID. I was also taught to always use homozygous positive and negative cells whenever possible. Sometimes of course it is not due to low incident/high incident antigens. I do know you need to use a homozygous cell when performing "rule outs". What is everyone else's practices and thoughts as I need to clarify our current antibody identification policy. Thanks in advance.
-
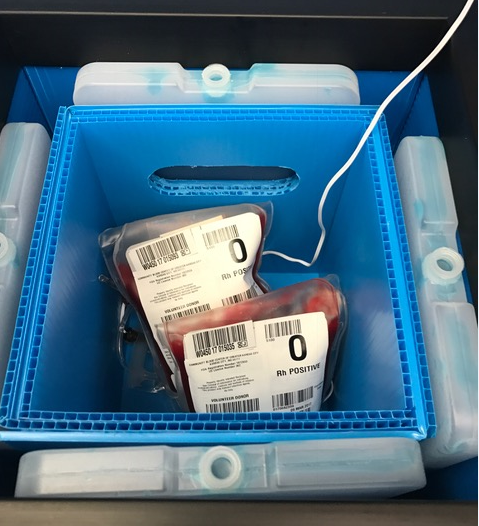
To clarify if we do issue more than one unit they are placed in a cooler with appropriate temp control. Also our coolers are validated for 24 hrs.
-
Hi I am creating a policy on issuing multiple units to one patient. We already do this for the ER, OR, CVICU, and ICU, and on any emergent need. But now we are getting requests for just general practice. Does anyone know of any AABB, FDA, or CAP standard about this I am having trouble finding one as far as who should and shouldn't get it. I am not in support of doing it just for non patient convenience thanks in advance.



Electronic crossmatch with Meditech
in Computer Systems / Software / ISBT128
Posted
You will need to go to the BBK History desktop and then to Replace XM Test. Under it you will need to enter the history record number and put a Y in the Exclude from Electronic Crossmatch. Their are of course steps in LIS and BBK parameters but the billing is on this page below.