Mabel Adams
Members
-
Joined
-
Last visited
-
Country
United States
Everything posted by Mabel Adams
-
blood warmer alarm temperature compared to temperature blood actually reaches
We use Ranger blood warmers in OR and sometimes other locations (but Belmonts for rapid infusion). I have been presented a question asking if we can still use them for blood because they warm the blood to 41C, but UpToDate says that blood shouldn't be warmed above 40C. I see no references listed in UPToDate to support their 40C requirement. We test the alarms on Ranger blood warmers, and they must alarm by 43C. From the Ranger Service manual: "The Ranger blood/fluid warming system is designed to warm blood, blood products, and liquids and deliver these at flow rates from KVO to 500 mL/min. At these flow rates, the device maintains fluid output temperatures ranging from 33°C to 41°C (Note: This is for room temperature fluids only). It takes less than two minutes to warm up to the 41°C ±1 set point temperature. The alert points on the Model 245 are 43°C ±1 and 46°C [+3, -2°C]." The 2002 AABB Guidelines for the Use of Blood Warming Devices says "The effectiveness of a blood warmer is limited by the flow rate of the infusion and the heating technology of the device in use. Most do not delivery normothermic (37C) fluids at very rapid flow rates--most reach a temperature of only 33 C to 36 C." These devices are FDA approved for blood transfusion, right? Can anyone supply an answer to the question of why (or why not) they are okay to use according to manufacturer's instructions, but UpToDate says not to warm blood above 40C?
-
Emergency or Massive transfusion in patient requiring irradiated blood
Almost all our platelets are pathogen reduced so they aren't much more of a worry than usual in an MTP. Does anyone know how likely TA-GVHD is in patients on drugs like fludarabine and cladribine? The inserts just say that the patients should get irradiated units, but I would guess that the risk is lower than someone 4 months post stem cell transplant. I've heard that TA-GVHD is 95% fatal, but I think that is in a recent transplant cohort. Bleeding to death is also fatal. The nuance is in the ED doc's perception of how likely it is that the patient is bleeding to death. Most of our irradiation patients are only candidates for transplant so I think their risk is small if they don't get irradiated blood in an emergency. They can probably postpone the transplant. In our most recent case at one of our small hospitals, I could see that the patient had no recent transplant and was not on those purine analog drugs so felt his risk was low and he did fine after getting 1 irradiated RBC and one non then going to IR to fix his second spontaneous splenic rupture in the setting of lymphoma and DOAC.
-
Emergency or Massive transfusion in patient requiring irradiated blood
If a small site that doesn't stock irradiated blood has to give emergency transfusion or a bigger place can't provide several rounds of an MTP that are irradiated, what are the risks? I know that patients who had a Stem Cell transplant in recent years must get irradiated products or face a very dangerous form of GVHD. I know that patients on purine analog drugs should get irradiated blood, but I don't know how dangerous it is if they don't. Otherwise, most patients seem to get irradiated because they are candidates for future transplants. Clearly, we can't let patients bleed to death but, if we get an MTP order on someone our system says needs irradiated blood, what do we tell the pathologist or ED doc about the risk? Our patient was a non-Hodgkins lymphoma who has not had a transplant, and I see no evidence of cladribine or fludarabine drugs in his list, so I think he is okay. I know that the doctors are the ones taking responsibility, but I want to understand the relative risks of various patient conditions with regard to GVHD.
-
Need Advice
Some of the worst hemolysis I have seen was in clostridium septicemia. Both cases were fatal.
-
Blind Samples/ Competency
Do you do anything to make them actually "blind", or do you trust your staff not to look up the original results?
-
Gel vs tube for DARA patients
Can we purchase this in the US yet? What company is making it?
-
Electronic crossmatch in ABO discrepancies?
Does anyone allow electronic crossmatch to be used in cases where a prior marrow transplant will never result in the usual reverse type on the patient (for example B to A)? We have a discrepancy blood type test in our computer that doesn't require the usual truth tables be met that we currently use for these patients. We require 2 separate specimens to be typed before we give any RBCs that aren't group O. We require 2 individuals to review any results turned out using the discrepancy test (this doesn't mean mistakes couldn't happen). We could have a patient with a cold agglutinin that would make an IS crossmatch incompatible (although maybe immunosuppressed patients won't make those?). I just want to see if anyone else has worked through all the logic involved in making sure patients are safely transfused yet the testing is appropriate to the need.
-
FDA requirements for 2 people to issue blood products for transfusion.
If you issue blood via a pneumatic tube system, this introduces some additional processes.
-
Gel vs tube for DARA patients
We sometimes find them negative in PEG. If that or a DTT treated screen is negative, we give units as electronic crossmatched (K matched if DTT used). Anti-CD38 is not a clinically significant antibody, and we have a negative DTT screen we can turn out which makes the computer happy.
-
Source of advice on transfusing patients with mismatched stem cell/bone marrow transplants?
We have patients that come home from university hospitals after transplants that we need to transfuse. We can often find in their charts the recommendations of the transplant center on what donor types to use. When we can't, I would like to have a definitive source on what blood type we should transfuse to these patients. The current patient was B pos, now A pos after a transplant 6 years ago. His chart says they consider him "cured". He forward types as A and back types as AB, as expected. I think we should be giving him A pos RBCs but I want a definitive source to cite in his notes.
-
Patient with anti-D, anti-C is negative with other reagent cells but incompatible with most units.
I expected to see a stronger reaction with the P1 cells labeled as "strong", but it does react with only the P1+ cells. Maybe P1 persists better on donor cells than reagent cells.
-
Cooler transport of cold stored platelets (CSP)
We need to determine how we will issue cold stored platelets in a massive transfusion. We would like to put them in coolers packed like RBCs, but we found that they get too cold. Has anyone identified a packing method that works well for CSP but doesn't mean we have to annually check 16 coolers by two different packing methods so we can use them for either CSP or RBCs? We may have to dedicate some coolers to platelets but would rather not.
-
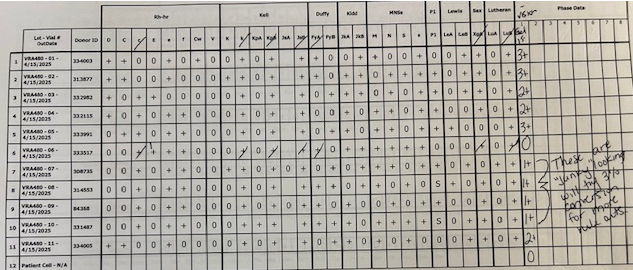
Patient with anti-D, anti-C is negative with other reagent cells but incompatible with most units.
The H explanation seems plausible although we didn't see much difference between A and O donors in terms of reaction strengths. I attached the original panel using Ortho 0.8% pre-diluted cells. Maybe these keep their H antigen better than the 3% cells we converted to 0.8%. The panel shown was only a few days from expiring. The 3% cells expire May 9th. This seems backwards from what we would expect if the antigens were weakening in storage. However, they are from different manufacturers and in different diluents. The 3% cells were from Immucor.
-
Patient with anti-D, anti-C is negative with other reagent cells but incompatible with most units.
That's a good question. The new sample was tested against Ortho 0.8% screen cells which were both positive due to her anti-D/C/G. Four C & D neg 3% panel cells were converted to 0.8% and run in gel with a 30-minute incubation. They were all negative. Then the new specimen was also used to crossmatch about 10 units, and we found 3 were compatible. I checked to see if she was getting TPN but don't see any. Sometimes that fats and proteins in the nutrition IV cause strange reactions. Usually, I have seen a positive DAT with it. If you can further describe the sort of protein you are thinking of, I would appreciate it.
-
Patient with anti-D, anti-C is negative with other reagent cells but incompatible with most units.
I noticed that pattern that suggests anti-G also. In transfusion, it doesn't matter whether it is anti-D/C or anti-G or a combination of them, right? We would pursue it in pregnant patients. Could she have been exposed to G without being exposed to either D or C? I feel like I've read that this is extremely rare, but not impossible. Yes, we find antibody to the diluent in Ortho's pre-diluted 0.8% reagent cells quite often. I believe that is what we found in the original testing besides the anti-D/C/G. When we make 0.8% suspensions from 3% cells, we use diluent 2 which lacks most of the antibiotics that are in the pre-diluted cells. It is a bit strange that the diluent antibody did not react with one cell. I have seen before where the antibody seems to have a predilection for some Rh antigens, and it seems like the antibiotic almost complexes with them on the RBC surface (maybe sterically). I think an antibody to the gel diluent explains why the panel went to negative except for with the D or C positive cells, Unfortunately, the reaction difference causing my consternation is between 3% reagent cells and donor cells suspended in the same diluent. If there were antibodies to the diluent that the 3% reagent cells were originally suspended in, I would expect those cells to react in gel rather than the donor units. I wonder if there is something in AS-1 that coats the RBCs to which this patient has an antibody. The negative reactions would then be due to lower levels in some donors compared to those eliciting stronger reactions. I had was told years ago that 3% cells freshly converted to 0.8% were somewhat more sensitive in Ortho gel testing, but this is acting in reverse. Also, I have heard that units are preserved to maximize their function after transfusion, not to stabilize antigens, whereas reagent cells are preserved to maximize antigen expression. Again, this is behaving backwards. I wonder if we should have done more antibody testing in PEG. Some specificities "like" PEG better than gel. Maybe we would have identified a 3rd antibody. It will be interesting to see if, in future testing, she makes another alloantibody. Appreciate this and any other input.
-
Patient with anti-D, anti-C is negative with other reagent cells but incompatible with most units.
We have a 42 y.o. Caucasian female with chronic anemia and cellulitis/sepsis needing debridement who has anti-D (2+) & anti-C (3+) by Ortho MTS gel. She was transfused elsewhere in 2021 and here in 2022, all Rh neg units. Two units each time. Screens were negative then. She has a history that suggests she may have shared IV drug needles at some point. I don't think there is a pregnancy history but not ruled out. She is A neg. Her initial testing in Ortho gel was clearly anti-D with C (could include G) but she had some 1+ reactivity with 4 of 5 D and C negative panel cells. The cell that didn't react was E+, D-, C-. Fya+, Fyb-, heterozygous for Kidd and MNS, but Lea- & Leb-. Auto control is negative. Three percent panel cells were then selected, diluted with Ortho diluent 2 to a 0.8% suspension and run in gel with a 30-minute incubation. By this method, we detected the anti-D and C antibodies in 2 cells that were D+, C- and 2 that were D-, C+ respectively. We were able to rule out all other typical specificities on 7 non-reactive cells and did not detect the weak reactivity previously found, suggesting that it was antibody to the pre-diluted 0.8% cells' diluent. One A neg, C neg unit was crossmatch compatible by gel that day and was transfused. Only that unit was crossmatched that day. Two days later (today), they requested more blood. All antiglobulin crossmatches in gel were incompatible--some units were A neg, some O neg. The reactions in gel were all 2+ or weaker with an atypical appearance of having one to two "stripes" from bottom to top, something we usually associate with cold reactive antibodies. Their strength appeared variable from weakly positive to 2+. We tried washing the donor cells, prewarming cells/plasma before combining them, 30 min. incubation in gel, and performing PEG XM's in tube which did not help. PEG was a bit weaker on the 2 units tested by that method (one the strongest reaction in gel and one the weakest), but still positive. We redrew the patient and got the same results with the new specimen. We did not test reagent cells by PEG. We ended up crossmatching about 20 A neg and O neg RBC units by gel and there were 3 that were truly compatible (not including the one from the first day). She got her second unit of this visit in the past few hours with no problems. What might cause reactions with AS-1 donor units but not with reagent red cells? Both are made up in the same diluent and tested by the same process. Some of the donor units were O cells like the reagent cells. Is there anything we should be considering? I expect she will be back for more blood in coming days to years (with our luck, probably with new alloantibodies since she is a responder who was transfused again). Thanks for your wisdom.
-
Does FDA require document control of forms or only procedures and records?
Thanks. That does seem like a good system. That brings up the next question. Does FDA expect every form to have an associated procedure? AABB does. TJC doesn't. Although we adhere to most of the AABB standards, we are no longer accredited by them so now I need to know what FDA requires.
-
Does FDA require document control of forms or only procedures and records?
I feel like the FDA requires that forms be controlled documents, but I can't find a regulation stating that. AABB includes forms in their definition of documents, but I can't find anything similar in the FDA regulations. FDA used to have a Guidance for inspections, but I can't find that either. Any pointers appreciated.
-
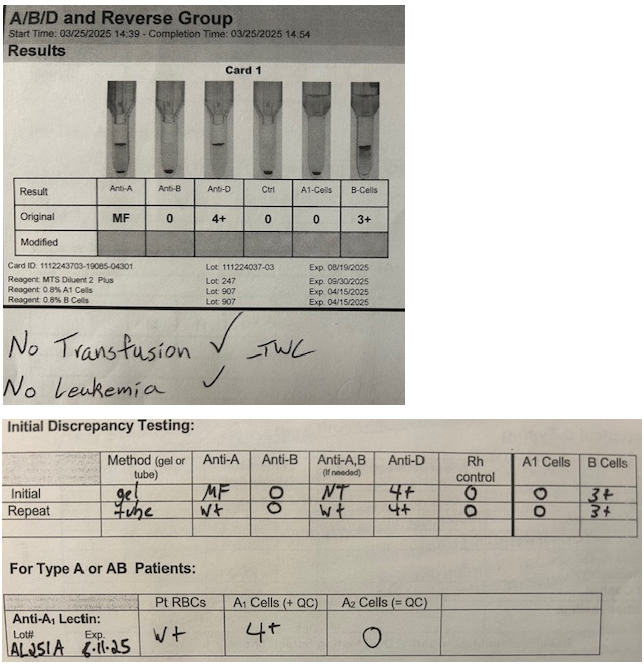
Unusual A type
We haven't tested any other antigens, although that would be interesting. Which would give us the most information? Her RhD looks typical. I know some Native American tribes have a higher percentage of R2R2. Maybe testing for E & C would be good? Also, I can't think how this additional testing will change how we manage this patient. Am I missing something?
-
Unusual A type
Confirmed no BM transplant, no history of leukemia, no recent transfusions, and not born a twin. She is Native American. We are calling her A pos and assuming she is a weak subgroup or chimera.
-
Unusual A type
Our repeat testing was on the CBC tube. I once had a phlebotomist reuse a tube that had a flash of someone else's blood in it so wanted to make sure more than one tube on the patient reacted the same.
-
Unusual A type
On repeat in another person's hands, the reactions I showed above as W+ were stronger and mixed field. The positive part came off like a big chunk that was 3-4+ (a bit weaker with the lectin) and the rest was a sea of free cells.
-
Unusual A type
What would cause these results? I don't expect the A1 lectin testing to look like the other tube testing in most weak subgroups that I know of. I also thought maybe the reaction with anti-A,B would be stronger. We are still getting answers to whether there may have been a marrow transplant. The leukemia question was about suppressed antigen expression. Chimera? What else? Patient is a pregnant Native American. I assume first trimester because this is initial prenatal testing.
-
Regulations on transfusion documentation
I found this in the AABB standards but can't find anything from a regulator that Nursing is guaranteed to think is definitive. 9.1, 7.5 Patient’s medical record: transfusion order, documentation of patient consent, component name, donation identification number, donor ABO/Rh type, date and time of transfusion, pre- and posttransfusion vital signs, the amount transfused, identification of the transfusionist, and, if applicable, transfusion-related adverse events
-
Regulations on transfusion documentation
Can anyone cite any regulations that stipulate what must be documented in an electronic transfusion record? I am looking at times when the usual electronic documentation wasn't used, and they manually document in a note or on a form that gets uploaded. I can't see any Joint Commission standards that state that they must document the DIN, product code, who transfused it and when. I see medication regulations for the time and "dose" which may apply because the FDA considers blood a drug, but nothing says specifically that they need to include the product code or even the DIN. This isn't the old days when paper transfusion records were returned to Blood Bank for record keeping.