Everything posted by AB123
-
ABO Grouping Discrepancies SOP
I'm currently in the process of reviewing our ABO grouping discrepancies SOP and currently we do not have anything in there for investigation of AB subgroups, does anyone have an SOP they would be willing to share that covers these investigations? or can recommend a good guideline or reference for this information? Thanks
-
Weak D test
Just checked the info and seems it does detect DVI, a bit sneaky of the rep to include this as extra when its not needed with the weak-D sera. "The blend of antibodies in this blood grouping reagent will directly agglutinate D positive red cells and may directly agglutinate red blood cells from most weak D and partial RhD including DVI. In addition the reagent will detect most partial D, and most weak D by IAT and, therefore, is suitable for RhD grouping of donor samples."
-
Weak D test
We have extra Sera for DVI as Ortho dont do a DVI+ cassette, so at the minute were are doing both Weak-D and DVI on the RH-D neg cords. I'm pretty sure the Weak-D also doesn't detect DVI.
-
Ortho Vision Cassettes in the USA
Asking out of curiosity, is the Vision in the US using glass bead cassettes or are they still marketing gel in the US?
-
Analyser Validation AABB
When I asked Ortho in the UK for a Validation plan back in 2015 when I validated the Visions they wouldn't provide one as they said it wasn't allowed under ISO, UKAS who undertake the ISO accreditation in the UK confirmed this and said "verification" as they call it is the customers responsibility and the supplier should be impartial. Interestingly out here in the UAE the vendors run most of the validation/verification tests then analyse the data for you and give you the report which ISO inspectors here seem perfectly happy with. So much for international standards!
-
Weak D test
Back in the days when we used to do blood groups in micro-titre plates manually, we always did the Du test as we called it then to pick up the weak D's. Since moving to gel technology in the beginning we picked up loads of D pos's that had previously been classed as neg due to the higher sensitivity of the Card methods. Since than I have worked at a few different labs and some have dropped the weak D tests and other have maintained them on newborns. I find the test a bit of a pain as the only time I find it positive now is when there is a positive DAT, I don't ever remember 1 occasion where the card D test was negative but the IAT D test was genuinely positive. Has anyone else who still does this test actually found a positive when the card Rh-d was negative?
-
Aliquot Labels
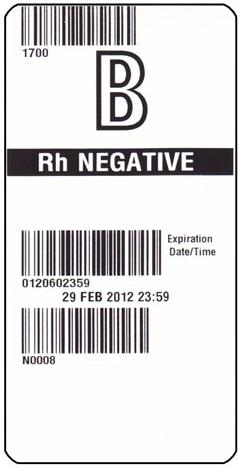
I thought the bottom barcode is probably product code, I was thinking maybe they didn't use ISBT compliant number due to copy write? But as you say no DIN would be a major issue both for compliance with ISBT standard and for checking procedures.
-
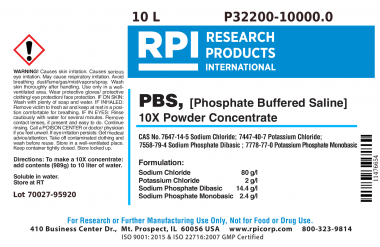
Making Own Buffered Saline
Thanks for reply How do you find the pHix? What Ph does it give? and do you ever have to adjust it? ?
-
Aliquot Labels
Currently we are using 4 x 4 labels for our aliquots as per ISBT standard. These are too big for our neonate bag and attaching them is messy. I have seen some examples of 4 x 2 labels been used that would be perfect size however I'm concerned about compliance with ISBT standard. Can anyone tell me if such labels are acceptable under ISBT128. I have checked the standards and it always referances the 4 x 4 label and there is not mention of 4 x 2. Also all examples of these labels I have seen are missing unit number. This seems like the most important number to me, how can it be dropped from the label? How can the checking process be completed without unit number been shown? Thanks
-
Making Own Buffered Saline
Does anyone make there own buffered saline? we have just switched to using the Ortho Vision and our local Vendor recommended normal saline not buffered. I have previously used the Vision in the UK and we were always advised to use PBS Ph7.2 and always did, so I was surprised by this advice. Since starting to use the Vision we have noticed a significant number of Cord blood samples with strong Pos DAT and Ctrl well positive, and C3 when checked with the Mono DAT card. When I asked the vendor regarding this he told me this was normal and to be expected, however I told him I don't believe it is as in my 2 previous years of using it I had never had a single case of this. I requested they contact Ortho regarding the issue and they came back with checking saline Quality/Ph! The Ph of our normal saline is 4-7 not within specification, the issue I have is that the only PBS I can get hold of here is for molecular biology use and around $100 a liter, as we are using about 150L a month this is not feasible. The ingredients to make PBS are cheap and its easy, or alternately we can just make the buffer to add to the saline. My concern is about QC and if we will have any issues from CAP/ISO,AABB etc. Just wondered if anyone else is doing this and if they have had any issues? Alternately I see Immucor make a product call Phix, that can be added to saline as a buffer, although more expensive this would be far cheaper than the PBS. does anyone use this product and have any feedback? There is also a powdered PBS product from a company called RPI which is the right specification and cost effective however they state that its a research product only, has anyone ever use this? Thanks
-
ORTHO VISION SALINE
We were provided the attached document by Ortho regarding saline specification. PH saline.pdf
-
Ortho Vision
I know this is a bit late but I have recently validated titer on the Vision and found it to have at most only a 1 titre dilution difference to Bio-Rad gel cards. Some higher some lower but most agreed. I was pleased with the outcome, just a little disappointing that the only result you get is "Done" and it doesn't give an interpretation hence manual interpretation and entry is required.
-
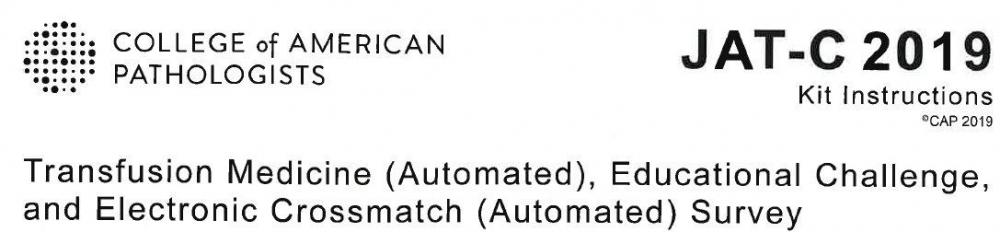
Ortho Vision CAP Specimens
JAT is the automated survey. I think J is a manual only survey. I wasn't really discussing simply asking if there are know issue with CAP samples on Ortho Technology, as certain technologies do have know issues with EQA specimens. As this analyser isn't in use yet we are reporting the results from the IH anyway.
-
Ortho Vision CAP Specimens
I carnt really see any other explanation for it and would be interested to hear from any other Ortho users who have this latest CAP. Yes the backgroup was clear on Diamed/Bio-rad and they too had a c Poitive A cell, I tried the same cells on Ortho and it was Poitive, then switched to a screened A cell that was c Neg and it was clear. I didnt panel the antibody but going off the screening cell result it can only be anti-c.
-
negative Cord DAT, positive eluate
It could be that the cells are coated but not sufficient to get a positive result. However when you perform the eluate on a large enough number of RBC'c the amount of IgG removed from these red cell's is then enough to coat and cause a positive reaction on the screening cells. Also the cells from the DAT will be heterozygous cells, hence you will get a stronger reaction from screening cells that are homozygous if sufficient antibody is eluted to coat them.
-
Ortho Vision CAP Specimens
JAT-C Got to the bottom of it with one of them, it was Anti-c antibody positive and was cold reactive with the A cells. Switched for some c- cells and now clear.
-
DVI
How common is DVI? Have done a google search but carnt find much information. Any sites that actually dual screen neonates or adults with both DVI+ and DVI- D clones? If so how often do you identify one if ever? Thanks
-
Analyser Validation AABB
I'm currently in the process of validating a new analyser, the Ortho Vision. I have validated this particular analyser before in the UK back in 2015. Now I'm working for a lab that is currently going through the process of AABB accreditation so I want to make sure I have covered all their requirements as this is my first experience with AABB. So far I have done comparisons, reagent on-board stability, carry over for antibodies (tested up to the Ortho claimed limit of 1:1024 titre), I also intend to do repeatability, running the same samples 5 times in a row to make sure the grading and interpretation is correct, the pathologist wanted 20 but I pointed out there is no way we will get 20 runs out of a transfusion sample. This is as much as I did in the UK and we had ISO shortly after and they were very satisfied with what we had done. As I have no experience with AABB I would like to hear from anyone who has gone through this process and has AABB experience. Is there anything I'm missing? Thanks
-
Ortho Vision CAP Specimens
I'm in the process of validating our new Ortho vision Analyzer and have just run our latest CAP specimens however I'm getting false positives on the back groups. Does anyone else use this analyser? are there any know issues with CAP specimens? Thanks
-
Titre Value
Currently our lab ignores +/-, 0.5, or weak positive results (depending what your technology classes them as) on titres, hence we only report the titre as the value that gives a minimum 1+ reaction. Is this usual practice? recently we are getting alot of +/- Anti-D's that are only giving very weak reactions in IAT but confirmed in the Enzyme, hence when titrated they dont meet the criteria to be classed as a even a "neat" so we report them as too weak to titre. Just wanted to check if this is standard practice as in my previous experience all titres were sent to reference lab and I never saw any report that wasn't at least a "neat" Thanks
- 2nd ABO
-
Change Control
In the UK the MHRA who are the UK equivalent of the FDA licence all blood facilities and hospital blood banks. One area they are very big on is change control. I just wondered how much the AABB focus on this area as at the moment our laboratory does not have a specific documented process for change control. Thanks
-
LIS Product Categories
Yes and this is what I've gone with, think its the easiest all round and the way I'm used to working. Thanks
-
AMR -AABB
Annual Management Review meeting. Although AABB just refer to it as scheduled management review in the standards, I've only ever know them to be done annually unless AABB expect more frequent?
-
Blood Issue Process
I wish, if I was I could make it 100 times better than what we have, its been designed by people who have clearly no concept of blood bank.