
Tabbie
Content Type
Store
Profiles
Forums
Blogs
Events
Frequently Asked Questions
Gallery
Downloads
Glossary
Links Directory
Questions
Jobs
Vendors
Posts posted by Tabbie
-
-
Thank you
So if you had an autoantibody and multiple clinically significant alloantibodies confirmed by phenotype (genotype if required) including let’s say for example anti-C you would not perform further exclusions for anti-Cw ?
-
Hi All
So if you had a patient with an auto antibody you would rule out all antibodies even clinically insignificant to confirm any underlying allo antibodies.
However if anti-Cw was detected you would ordinarily give crossmatch compatible BUT you are giving antigen positive units due to auto so crossmatch would positive ?
Therefore what do you do ? crossmatch anti-Cw negative units ? Realise not clinically significant but ordinarily if crossmatch was positive you would not give that unit to the patient? You would select another unit.
Thanks
-
Your a star Malcolm as ever complex but clear and reference to the GATA-1 gene to compare scenarios, putting it into perspective.
Much appreciated
-
On 8/22/2018 at 9:30 AM, Malcolm Needs said:
No, you are not thinking about this wrong, but, if there is an IgG antibody present that is diluted out at one in two, it is not going to be of any clinical significance in that particular episode of transfusion, and in particular as it is a "warm" auto-antibody, as most "warm" auto-antibodies are directed against a very high prevalence antigen (such as Rh17 or Rh18), even though the antibodies tends to mimic specificities such as anti-E or anti-e, and so you will be unable to provide the required D--/D-- or Rhnull red cells that would be the only red cells properly compatible.
Hi Malcom
When you say mimic does that mean that the patients phenotype would not be E+ or e+ which would be the case if it was just an auto anti-E (wondering about how sometimes phenotype is not the same as genotype). Or would you not know until you performed adsorption/elution with D—/D— to confirm the Rh17.
Thanks
-
Hi All
So if a patient who is a D Variant (weak/partial) that can produce Anti-D is subsequently immunised with D positive RBC. The auto and DAT would be negative usually ? However anti-D causes extravascular haemolysis so DAT should be positive. Is anti-D produced from a D-Variant any different in strength/avidity. Realise that pos DAT can occur for other reasons AIHA etc.
Can anyone explain the mechanism of the anti-D anomaly? Or a link to an article ?
Thanks
-
Great thank you 😀
-
Hi All
Would anyone have a method for this neutralisation technique ?
Thanks
-
Thanks Galvania
All made up so if you don't ever see something I have 'made up' please let me know. I was trying to fit lots of questions into one scenario.
-
 Thanks for your time yes very helpful. I will keep read
Thanks for your time yes very helpful. I will keep read
-
So for example the question below
If you only knew that the patient had been transfused but no other details how would you phenotype or would you just obtain a genotype?
The BSH guidelines say " If the patient is known to have been transfused in the previous three months, phenotyping may be misleading"
Most regularly transfused patients such as Haemoglobinopathy patients admittedly would already be phenotyped but if they were not they would required Rh K matching units, DARA patients would you Rh phenotype if units are required ASAP but you have time for a crossmatch.
What further tests would you do if you had the resources to ensure you provided matched units
So for example after the elution to identify the antibodies can you use the RBC left from the process to phenotype ? or does the elution damaged the RBC is there another procedure for phenotyping if the patient has been recently transfused?
Misleading means ? - What anomalies would you actually see ? weakened reactions, dual populations (if ABO) anything else?
Why with warm autoantibodies does elution not help ? What about in pregnancy are there any anomalies with elution/adsorption/phenotyping ?
Thanks
-
I work in a small lab we just don't get the experience of the unusual. I am trying to learn more by posting hypothetical case studies as I cant post real ones.
Thanks
-
Great thanks Galvania
More questions

If it was an anti-I would the pattern be pan-reactive by IAT weaker and Enzyme stronger reactions?
If patient was previously transfused would you phenotype RBC if you knew the group of the ABO mismatch i.e. if a dual population say Group A given to a group O? Would you perform an eluate to remove the antibodies then add anti-A to remove the A RBC then phenotype the O RBC and assume they are the patients RBC as the phenotype?
If you only knew that the patient had been transfused but no other details how would you phenotype or would you just obtain a genotype?
If no mix field and DAT C3d only and Donath Landsteiner test was positive would you then titer with P antigen positive RBC?
Cheers
-
Thanks Malcom for reply it was a while ago and I didn’t cite it as I thought I would come across more that would explain it. But looks like from you reply this is not possible. If I come across it again I will post.
-
-
Hi All
Lewis antibody exclusions.
Realise they are rarely clinically significant only causing HTR and would perform crossmatch compatible. However I want to clarify the theory for exclusions.
Human Anti-Lea is found in Le(a-b-) however exception to rule in Tawain where 10 Lea (a-b+) patients with anti-Lea were found. Most anti-Lea contains weak anti- Leb causing false positives.
However monoclonal reagents seem to indicate no cross reactivity? What reagents do you use to exclude the presence of either anti-Lea or Leb ?
Thanks
-
Hi All
Reading about an auto anti-C with C antigen negative expression by serology phenotype and genotype. If you could not obtain a result from auto adsorption (not enough sample to test) how would you confirm it was an auto antibody ?
Thanks
-
I like things to be right keep up the good work of correcting and educating 😀
-
Patient phenotype is Fya + Fyb+
I just had not seen a Gata mutation result before had read about it. Thought it may be an additional molecular phenotype request but it was included in the panel reported
-
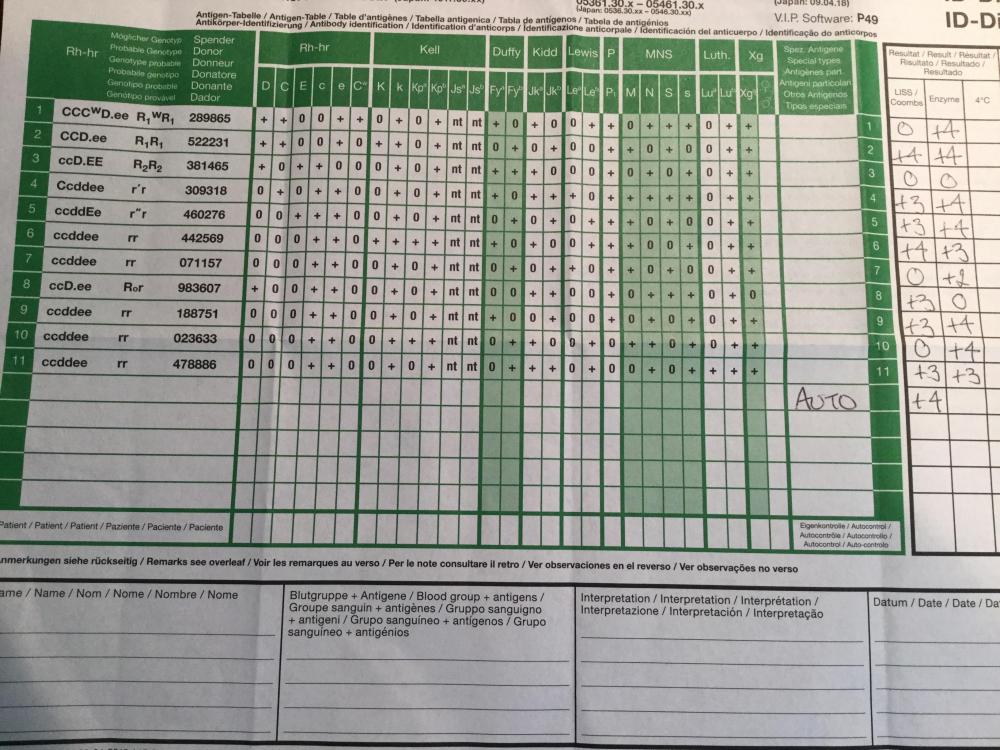
Final results
Auto Anti-Jka and nonspecific enzyme IAT ( no requirement to select Jka antigen negative units)
Phenotype E-K- and again Fy GATA mutation negative.
Has anyone seen an anti-Jka only react by enzyme and not IAT which has not been an auto anti-Jka ?
Thanks
-
Final results ABO group not determined.
Phenotype c-E-K-M+N- and interestingly Fy GATA mutation negative.
-
Are there any rules for ruling out P1 with the different antigen expression strengths?
Thanks
-
9 hours ago, Eagle Eye said:
Was elution done? Anti-c may be IgM!
(we do see this when reverse cells giving discrepancy due to (mostly) cells being M+/Lea+/Leb+ , some time c+.
Interesting about Lea+Leb+. The eluate was negative
-
Hi All
Female patient not childbearing age with historical A POS no antibodies detected subsequently multi transfused.
After transfusion of 2 x O NEG units a week later a sample tested no antibodies detected by IAT however cross-match request was performed by IAT and both units were positive
Further testing
DAT +1 and panel cells enzyme ONLY reactive +2 with R1R1 cells and the rest of the panel cell reactions +4
ABO reverse grouping showed A cells +2 (conclusion therefore possible A subtype with a no specific antibody or reaction with cde in reverse grouping reagents due to an anti-c)
Reference Lab Results
Non specific anti-E and anti-c detected in enzyme IAT, DAT IgG 1+
As multi transfusion advise was cross-matching group O E-c-K- red cells
Genotyping results to follow.
Would anyone agree with the reactions with the reverse grouping agents and if they have seen this was the anti-c detected been by IAT/and or Enzyme
Thanks
-
Hi All
Historical A POS (never phenotyped) no antibodies detected. MDS patient, multi-transfused with APOS/NEG units over past 3 months.
Results
Screening cells (using BioRAD 3 cells) +2 positive reaction only with R2R2 (cell II). DAT +2 (IAT method/ IgG/C3d polyspecific)
Panel negative which suggested a low prevalence/frequency/incidence antibody however - crossmatch was positive which led the question was there was another underlying antibody ( a soup of antibodies).
Reference Lab Results
Possible Jka by IAT enzyme and non specific enzyme reactions. Now awaiting genotyping.
Advise to crossmatch Rh/K/Jka D-C-E-Jka-
My question is now the patient has returned to group A POS (there was a dual population before with the D type due to the previous transfusions)
is it acceptable to transfuse D+ (as historically RhD+) C-E-Jka- units or could there be a potential D typing anomaly ?
Thanks


antigen negative units for patients with autoantibodies?
in Transfusion Services
Posted
Yes I should have added allo anti-C.
Also thought may be anomaly if both allo anti-C and allo anti-Cw were detected like ceppellini effect but there is not.
Thanks for clarity