
Carrie Easley
Content Type
Store
Profiles
Forums
Blogs
Events
Frequently Asked Questions
Gallery
Downloads
Glossary
Links Directory
Questions
Jobs
Vendors
Posts posted by Carrie Easley
-
-
-
If at all possible, define a pre-admission process so that a T&S can be drawn prior to the day of surgery. No one is happy when they find-out that the patient on the table has an antibody that will significantly delay packed cell availability. I would also "make friends" with your Perfusion team. Ours are the TEG experts in the OR, and help to guide the component utilization. We still reserve two platelets for a CAGB, but rarely transfuse these patients.
-
On 10/14/2019 at 10:20 AM, slsmith said:
Right now we are using Radsure but are going to switch to RAD Control(made by TYPENEX). It is a smaller label and stored at room temp rather than the refrigerator. The thing everyone likes about it is the lot number and exp date that we write on the irradiation log is actually a sticker on its own that you peel off and attach to the log. As far as a making doses from the parent bag we use a ISBT based label that has irradiation printed on, like Malcolm's.
Just FYI... RadSure can now be stored @ RT.
-
On 10/25/2019 at 12:02 PM, Mabel Adams said:
What will you be using for the billing HCPCS code for liquid plasma? I don't see one in the latest CMS reimbursement list that I have.
The code is P9044. It's about 25% more than frozen plasma from our supplier.
-
We are a level II trauma center that averages 4-5 MTP's per month. We have an order set built in our hospital information system that includes baseline labs, hourly labs, TXA bolus/infusion, and eight rounds of blood components (48 packed cells, 48 plasma, 8 plateletpheresis, and 70 units cryo). The components cross to our BB LIS (SoftBank). We issue rounds until told to stop by patient care staff. We either select/issue or emergency issue based on how much of our compatibility testing is completed. Although we use the Epic blood product administration module (BPAM) for most transfusions, it's currently too clunky for MTP. We issue paper transfusion records generated by SoftBank for the RN's to document on. These are returned to the Blood Bank so that we know what was given & when. Any missing documentation is included in the comprehensive review that takes place after each event.
-
2 hours ago, PBM RN said:
Carrie,
We require two separate draws on any patient without a historical ABORH on file, and we pull a T&S on most OB patients when they are admitted per OB hemorrhage risk. However, we have recently built and add-on for a Blood Bank hold tube that is run in ED as a part of the Rainbow draw. This may be similar. Let me know and we can pass the build along.
We have a similar policy. We only request the second draw if they order packed cells w/ historical type, though. Our high-risk deliveries also get a type and screen. My issue is when we need to turn the ABRH specimen into a full T&S (adding the ABSN to the existing order). We have not found a way for Epic to automatically add-on to a BB specimen like they can in other areas. We also have a BB Hold tube, but the issue is the same...if they order testing, we have to manually go in to Beaker & add collection info. Has anyone found a true add-on method that interfaces f/ Epic to Soft?
-
New question

Does anyone have a good workflow for adding an antibody screen onto an existing ABRH? We frequently run into this in our L&D (ex. Mom comes in planning for a vaginal delivery, so they order an ABRH. She turns into a C-section, so they want a full T&S). Since Epic sees Softbank as a reference lab, we can't get the add-on without the banker manipulating in Patient>Orders>Modify. I'd appreciate any insight!
~Carrie
-
2 hours ago, ninachka224 said:
Hi Carrie,
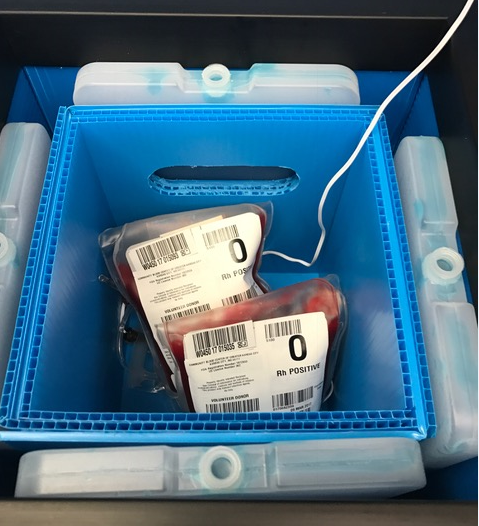
Can you please tell me where you got the empty blood bag?
Thank you,
Nina
They are just 400 mL transfer bags made by Charter Medical. Item # T3104
-
Same here...straight to K-B if no infant Rh available.
-
Me
 We use Epic/Beaker with SoftBank.
We use Epic/Beaker with SoftBank.
-
5 hours ago, kelliott15506 said:
Will you be willing to share the Journal Reference(s) that supports(s) your policy?
- Chhibber V et al. Is group A plasma suitable as the first option for emergency release transfusion? Transfusion 2014;54:1751-5.
- Cooling L. Going from A to B: The safety of incompatible group A plasma for emergency release in trauma and massive transfusion patients. Transfusion 2014;54:1695-1697.
- Isaak EJ, et al. Challenging dogma-Group A donors as universal plasma in massive transfusion protocols. Immunohematology 2011;27:61-65 (NOTE: Free pdf download of full issue).
- Mehr CR, Gupta R, von Recklinghausen FM, et al. Balancing risk and benefit: maintenance of a thawed group A plasma inventory for trauma patients requiring massive transfusion. J Trauma Acute Care Surg 2013;74:1425-31.
- Zielinski MD et al. Emergency use of prethawed group A plasma in trauma patients. J Trauma Acute Care Surg 2013;74:69-75
Some of these are several years old. A quick search will literally provide dozens of articles. It was well publicized @ AABB 2018 and the Blood Bank Guy has a podcast from August 2017 that provides more info.
-
Just got the book today (as well as the positive DAT work-up counterpart)! Looking forward to incorporating these case studies into new employee training.
-
We use type A liquid plasma (never frozen) for traumas and massive transfusions until type-specific/compatible can be thawed.
-
-
An amazing honor and well-deserved. The knowledge you share spans continents and grows exponentially!!!
-
That’s awesome Mabel! Is this workflow just in OpTime, or can it be used in other settings?
-
On 7/3/2018 at 10:09 AM, Baby Banker said:
We have dedicated blood bankers on each shift. This was suggested to us by an FDA inspector. We supplement with generalists on evenings and nights.
Interesting! Could you please share the size/complexity of your transfusion service?
-
37 minutes ago, Jessica A said:
We are going to Softbank and I really wish hospital administration would seriously consider purchasing the SoftIDTX module which works similar to BPAM but WAY better. For example, it looks a lot more like the anesthesia BPAM module than the nursing BPAM module. You can see every unit available for the patient on one screen and simply click "start" or "stop" when you begin and end the transfusion. It does a better job of prompting for vitals as well. It would work fabulously well in an MTP situation.
For those of you who don't use BBID armbands, how do you meet the CAP requirement for a secondary method of patient identification? I get that rover does the ID at the time of draw and BPAM does it at the time of transfusion but do we just get a pass for MTP situations? As I brought up with EPIC and nursing, it is not out of the realm of possibility to have 2 MTPs going at the same time who are different blood types. This terrifies me.
For those that DO use BBID armbands, how do you get EPIC to acknowledge the armband as a patient identifier? Can they add a field in BPAM to scan or type the armband number and bounce it back to something? I feel like we need to keep the BBID armband for MTP situations since I will have literally nothing else to make sure the correct patient gets the blood.
We are also Softbank/Epic users. We currently use a BB armband for alias patients, but are moving away from it. Even with patients admitted with an alias, we have at least three unique identifiers without the BB armband. The patients are rapidly admitted with a unique, pre-built, never to be repeated alias name, an MRN that will stay w/ them the entire admission (merged to a prior MRN after discharge if applicable), and the CSN/stay number that stays with them throughout the admission. These pieces of info are on hospital armband, specimen labels, transfusion records, and all compatibility labels. Even after MRN's are merged, you can search for the alias MRN and it will take you to the actual MRN. It's all extremely traceable. We have experienced multiple traumas and MTP's simultaneously.
I was told that Epic does not offer a field for the BBID.
-
3 hours ago, John C. Staley said:
Wow, out of the business for a couple of years and I don't have a clue what most of the acronyms in this thread mean!!

Malcom is, of course, correct. Epic is a hospital information system/electronic medical record. They have a laboratory module called Beaker, but do not have a blood bank information system. Epic users have to integrate a stand-alone B.B. system (Meditech, SoftBank, Sunquest, etc...) with it. Epic has a blood product administration module (BPAM) that allows electronic scanning of patient and unit at the bedside (in lieu of paper records). It’s not really fast enough for a massive transfusion situation at this point so we struggle to find an alternative in the most stressful times. Rover is a handheld device that phlebotomists use for positive patient ID and real-time collection label printing.
-
We are an Epic user and use BPAM for everything but MTP, Trauma, and uncrossed units. Surgery is an interesting hybrid of paper and OpTime (Epic anesthesia module). I chair our MTP committee, and BPAM is simply not fast enough for rapid administration at this point...it basically creates a flow sheet of documentation for every unit. I’ve seen a mock of an MTP module, but so far it’s only for Op Time (not trauma bay, L&D, EMD, cath lab, etc...) We have, however, created some ways to get the units documented on paper into the patient’s I/O.
We don’t use Blood bank bands for most patients, but were still using for patients admitted with an alias (most trauma admissions). We are about ready to discontinue in that setting as well. Rover is a great thing!
What B.B. system are you on? I’m happy to share all we have learned the hard way. Message me, and maybe we can find a time to chat?
-
29 minutes ago, MOBB said:
I'll apologize in advance for the lengthy answer.
I had always been taught that matching Rh and Kell were helpful in preventing alloimmunization for SS patients, but I attended a lecture by Dr. Gehrie last week on this topic and he had a very different opinion. I'm looking forward to discussing this with my medical director-it's so different from everything I've previously read.
Dr. Gehrie said the 2014 NHLBI Expert Panel made a moderate recommendation based on low-quality evidence that RBC units that SS patients should include matching for C, E, and Kell antigens and that serologic antibody matching programs results were varied. He also advocated that only 30% of SS patients form alloantibodies which makes studies difficult-patients may not have made antibodies, but maybe they are part of the 70% that wouldn't make antibodies.
He shared the Chou et al 15 year retrospective analysis from Children's Hospital of Philadelphia. The patients were provided D, C, E, and K matched RBCs from mainly african american donors.
N=123 chronically transfused, N=59 episodically transfused.
58% of the chronically transfused and 15% of the episodically transfused were alloimmunized.
91/146 antibodies were to Rh antigens.
The biggest takeaway for me was 87.6% of the patients had Rh variant alleles which help explains the alloimmunization rate.
Dr. Gehrie's protocol at Johns Hopkins is to do nothing for SS patients until they form an antibody, then genotype the patient and provide matched products based on the genotyping.
I was there as well! He was an excellent speaker. We should find a way to post when there is an upcoming B.B. event so that some of us may meet in real life.
-
We match Rh/K/Fya for all peds SS patients and all adult SS patients who have made at least a single RBC alloantibody. We make every effort to send warm autos for RBC genotyping and match everything we reasonably can. Our blood supplier maintains an online antibody registry for their customers, so it helps with continuity of care if people hospital hop (assuming all customers utilize it).
-
On 5/2/2018 at 5:17 PM, csjuarez said:
We use the Soft LIS system. Our pre-admission outpatient specimens are extended for 14 days if the patient hasn't been pregnant or transfused in the last 3 months. We are able to update the expiration date for the sample in Patient -> Orders -> Modify when we are reviewing the patient's history and receiving the specimen in the Blood Bank. The expiration is automatically set at 3 days for all patients, so the tech receiving the specimen makes the change manually.
Virtually same workflow. We set for 3 days post-op; maximum 14 days from draw as long as not pregnant/transfused in last three months. Our latest upgrade (25.3.1) automatically resets outdate if patient happens to get a packed cell in that pre-op window.
-
9 hours ago, Darren said:
We use the FetalScreen II from Ortho/Quotient. Reading through the instructions for use makes me wonder if it's useful at all. I think we may consider some send out options for KHB or flow cytometry and relieve the bench staff of the effort altogether.
The fetal screen definitely has its place...just not for antepartum bleeds (at least the kits I’m familiar with). I keep hoping our Hematology department will bring flow in so we can ditch the K-B!!!

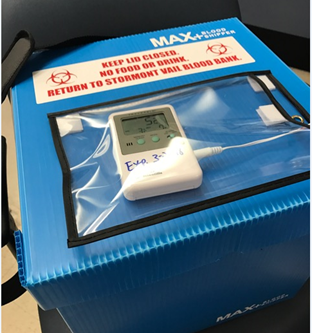


Blood Product cooler thermometer
in Transfusion Services
Posted
It’s a two component epoxy.