Leaderboard
-
in all areas
- All areas
- Records
- Record Comments
- Record Reviews
- Jobs
- Jobs Comments
- Jobs Reviews
- Questions
- Question Comments
- Question Reviews
- Links
- Links Comments
- Files
- File Comments
- File Reviews
- Images
- Image Comments
- Albums
- Album Comments
- Records
- Record Comments
- Events
- Event Comments
- Blog Entries
- Blog Comments
- Topics
- Posts
- Status Updates
- Status Replies
-
Custom Date
-
All time
June 28 2007 - April 20 2024
-
Year
April 20 2023 - April 20 2024
-
Month
March 20 2024 - April 20 2024
-
Week
April 13 2024 - April 20 2024
-
Today
April 20 2024
-
Custom Date
03/30/2019
-
All time
Popular Content
Showing content with the highest reputation since 03/30/2019 in all areas
-
Mock-up cases
Andrea Pointer and 18 others reacted to Bb_in_the_rain for a topic
For those of who works in transfusion service laboratory and would like to learn more reference cases, I can post some mock-up cases here. If you would like me to do it, please hit the "heart" button on this post. If enough folks want to practice case studies on reference lab cases, I can post mock-up cases here weekly or so..19 points -

Storing Saline Cubes
jshepherd and 16 others reacted to John C. Staley for a topic
I'm going to be blunt. This is ridiculous!! You have the potential of causing far more problems by removing the cubes from their protective container.17 points -
All, I am about to blow your mind.... Our plasma freezer is down and so is our backup. The freezer will not get colder than -18 C. I was preparing to move all the products into boxes with dry ice until I had a conversation with my 87 year old dad, a retired blood banker from University of Chicago. He said to me, do not take the plasma out of the freezer and put it in boxes, PUT THE DRY ICE IN THE FREEZER, IT IS THE BEST STORAGE BOX YOU HAVE!!!! MIND=BLOWN!!!! I did that. Our freezer is currently reading -25.1C and getting colder. Furthermore, the probes in the freezer continually monitor the temp in the freezer so you don't have to record temps every 4 hours, the chart is doing that for you!!! Isn't that cool? That perfectly illustrates the difference between wisdom and knowledge there. I wish we could hire my dad. I just had to share this here. PS. Freezer is now at -26.4C.12 points
-
You did everything that was required in this situation. The patient was a trauma and needed emergency transfusion. The risk of death outweighed the risk of a hemolytic transfusion reaction in that scenario, according to the treating physician. I once had a trauma surgeon tell me "I can treat a transfusion reaction but I can't treat death!" That put things in perspective for me. That is why thy sign the consent. Next step would be to report this to your risk management department so that follow-up can be made, including monitoring the patient for the s/s of DTR.11 points
-

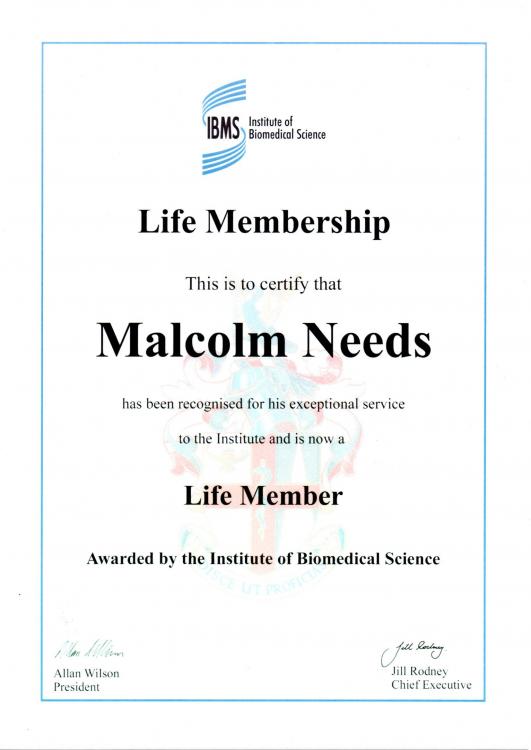
Life Membership of IBMS.
SbbPerson and 10 others reacted to Malcolm Needs for a topic
11 points -

Transfusing Blood in the OR
Carol Salo and 10 others reacted to John C. Staley for a topic
This is not a popular concept but at some point we have to accept there are things we can not control. Once the blood leaves the blood bank we are at the mercy of other humans and as long as the human factor is involved there will be human error be it unintentional or intentional. Attempting to complicate a process will only provide inventive humans the opportunity of coming up with creative work arounds to circumvent your best of intentions. At some point you just have to step back, do your job and hope for the best. I had a corporate transfusion QA director who could not accept that human error could not be completely eliminated with out eliminating human involvement in the process. Her directives became horribly complex solutions with multiple, redundant checks and balances only resulting in increasing problems. Bottom line, pick your battles and fight those you have a reasonable chance of winning. Make suggestions, offer insight, provide training opportunities but at the end of the day realize that you have to accept some things are simply beyond your control and even your influence. On that happy note I'll step off my soap box and stop my philosophical ramblings.11 points -

CORD BLOOD NOT MATCHING HEEL STICK TYPE
Eman and 10 others reacted to Malcolm Needs for a topic
If you put a drop of blood on something like a filter paper, and then add a drop of 1M NaOH, if it is adult blood, after a couple of minutes it will turn a sort of yellow/brown colour, as the Hb is denatured by the alkaline, whereas, if it is blood derived from the baby (including cord blood), the red cells will stay red, as HbF is not denatured by the alkaline for much longer. It is rather like doing a Kleihauer, but by "bucket chemistry", as it is known!11 points -

Gold Medal.
Ally and 9 others reacted to Malcolm Needs for a topic
I am enormously honoured to announce that I am going to be awarded the Gold Medal of the British Blood Transfusion Society at their Annual Scientific Meeting in Brighton this year. It is awarded to an individual for their exceptional and long standing services to the Society and to the practice of blood transfusion in the UK. Sorry if this sounds egocentric, but I am very excited.10 points -

Do you antigen type for the entire group?
SbbPerson and 9 others reacted to Malcolm Needs for a topic
When I was working in the Reference Laboratory at the NHSBT and, come to that, when I was working for a short time in a Hospital Blood Bank, we would ALWAYS test for the C, c, E and e antigens, together with the K antigen, both for patients and donors, and we would also test for the antithetical antigen, as well as the cognate antigen (in other words, as in your example, the Jk(a) and the Jk(b) antigen. We ALWAYS did this, except when the grouping reagent was exceedingly rare (e.g. anti-Dib) or the antibody AND the antigen were extremely rare (e.g. anti-Kpc). The reason we did this, particularly in the NHSBT Reference Laboratory, was because we wanted to identify very rare phenotypes, such as Kp(a+b-), or even rarer (in most cases), null phenotypes, but there was also a paper that showed that people who were transfusion dependent, such as sicklers and thal patients tend, once they have made an initial atypical antibody (particularly anti-C, anti-c, anti-E, anti-e or anti-K) to make all sorts of specificities (I'll try to look up the paper and get back to you on here). Other papers comparing their findings actually agreed with them. I say ALWAYS, but then, of course, the Bean Counters, who know nothing about Blood Group Serology, or about Patient Requirements, and care even less, came along, and we were banned from doing this as, apparently, IT COST TOO MUCH MONEY, except in special circumstances, such as patients from the Black populations, where we were privileged to be able to test for both Fya AND Fyb, in case they were Fy(a-b-) - and, of course, most of those who were found to be Fy(a-b-) had the FYB gene, so would very rarely produce an anti-Fy3, as they were homozygous for the GATA1 gene mutation. Unfortunately, what these "suits" seem to forget, despite counting beans for a living, is that, if the patient goes on to produce other, clinically significant, atypical alloantibodies, they will occupy a hospital bed for longer while suitable blood is identified, including, sometimes, cryopreserved units, ALL OF WHICH IS FAR MORE EXPENSIVE THAN THE INITIAL TYPING WAS IN THE FIRST PLACE - but what do we professionals know! RANT OVER!!!!!!!!!!!!!!!!10 points -

Immune checkpoint inhibitor drugs can cause DAT negative AIHA
donellda and 9 others reacted to Mabel Adams for a topic
We had a melanoma patient on Nivolumab = Opdivo who apparently has hemolytic anemia but his IgG was only microscopically positive and his complement was negative. Hgb 5.5. Retic % slightly elevated, absolute retic normal, immature fraction retic very high. Bili and LDH normal. Hpt <14 and responded to steroids. They blamed this drug so I hunted up this article. This was new to me so I wanted to share it. Clinical Trial Am J Hematol 2019 May;94(5):563-574. doi: 10.1002/ajh.25448. Epub 2019 Mar 13. Clinical and laboratory features of autoimmune hemolytic anemia associated with immune checkpoint inhibitors Rebecca Karp Leaf 1, Christopher Ferreri 2, Deepa Rangachari 3, James Mier 3, Wesley Witteles 4, George Ansstas 5, Theodora Anagnostou 6, Leyre Zubiri 1, Zofia Piotrowska 1, Thein H Oo 7, David Iberri 8, Mark Yarchoan 9, April K S Salama 10, Douglas B Johnson 11, Andrew D Leavitt 12, Osama E Rahma 13, Kerry L Reynolds 1, David E Leaf 14 PMID: 30790338 DOI: 10.1002/ajh.25448 Free article Abstract Immune checkpoint inhibitors (ICPis) are a novel class of immunotherapeutic agents that have revolutionized the treatment of cancer; however, these drugs can also cause a unique spectrum of autoimmune toxicity. Autoimmune hemolytic anemia (AIHA) is a rare, but often severe, complication of ICPis. We identified 14 patients from nine institutions across the United States who developed ICPi-AIHA. The median interval from ICPi initiation to development of AIHA was 55 days (interquartile range [IQR], 22-110 days). Results from the direct antiglobulin test (DAT) were available for 13 of 14 patients: 8 patients (62%) had a positive DAT and 5 (38%) had a negative DAT. The median pretreatment and nadir hemoglobin concentrations were 11.8 g/dL (IQR, 10.2-12.9 g/dL) and 6.3 g/dL (IQR, 6.1-8.0 g/dL), respectively. Four patients (29%) had a preexisting lymphoproliferative disorder, and two (14%) had a positive DAT prior to initiation of ICPi therapy. All patients were treated with glucocorticoids, with three requiring additional immunosuppressive therapy. Complete and partial recoveries of hemoglobin were achieved in 12 (86%) and 2 (14%) patients, respectively. Seven patients (50%) were re-challenged with ICPis, and one (14%) developed recurrent AIHA. Clinical and laboratory features of ICPi-AIHA were similar in DAT positive and negative patients. ICPi-AIHA shares many clinical features with primary AIHA; however, a unique aspect of ICPi-AIHA is a high incidence of DAT negativity. Glucocorticoids are an effective first-line treatment in the majority of patients with ICPi-AIHA, and most patients who are re-challenged with an ICPi do not appear to develop recurrence of AIHA.10 points -
I think you should invite members of that committee to remove a bag from its cube, try to label it sufficiently (substance, lot #, expiration, etc.), attach that label in such a way that it will stay attached when the bag 'collapses' as it's emptied, hoist the bag up to the level of a cell washer without the aid of the box (especially this part), and suggest ways to keep the collapsed bag at an angle that will ensure all the contents are used. I'm willing to bet they'll come around.10 points
-

Serological Crossmatch when providing Antigen Negative units
AuntiS and 9 others reacted to Malcolm Needs for a topic
No, there is a lot more to it than that. Anti-A and anti-B are isoantibodies, rather than alloantibodies. In other words, they are "naturally occurring" and do not have to be stimulated by either red cell transfusion or pregnancy. They are usually stimulated by particles in the air (including human cells that have been shed into the air) that either express chemical compounds that mimic the A and/or B antigens or, in the case of shed human cells, actually do express these antigens (remember, the A, B and H antigens are histoantigens). On the other hand, genuine alloantibodies (for example, let's say an anti-Jka) that are stimulated by transfusions and/or pregnancy, have, by definition, shown the individual to be a "responder". It is by no means unusual for an individual who has produced a genuine alloantibody (such as the anti-Jka mentioned above) to produce an alloantibody of another specificity (or alloantibodies of other specificities). Such other alloantibodies may not be easily detectable by routine serological techniques for various reasons. Three of these are that the antibodies may not become serologically detectable at the same time (one may be detectable as early as the other, as not all antibodies "read the books"), that an antibody may be evanescent (or "disappears" from the circulation quite quickly - such as many Kidd antibodies - but these can remain clinically significant if re-stimulated), and thirdly, that the cognate antigen is not expressed on either the screening red cells or the red cells used in the antibody identification panel (for example, in the UK, to give two examples, the Jsa antigen and the Wra antigen, and both of these antibodies can be exceedingly clinically significant). For this reason, it is very important that a serological cross-match is preformed (and found to be compatible), even if the blood provided is antigen negative for a known cognate antibody. You may well ask, "Well, what about an anti-Wra (for example) that is present as a monospecific antibody? Is that not clinically significant?", and the answer is "Yes"! Indeed, there was a fatal case of an acute transfusion reaction caused by anti-Wra within the last decade in the UK, and the court decided that it was death by misadventure, because anti-Wra is known to be quite a common antibody, whereas the cognate antigen is sufficiently rare for the Law to recognise that it does not need to be expressed on screening cells (otherwise the Reference Laboratories would be overwhelmed with samples that have anti-Wra in their plasma/serum - and this is only one such specificity). This may be one of the few times that our judiciary have used their brains (did I say that??????????!!!!!!!!!!!!!!!!!) and the decision may have been influenced by an editorial in Transfusion, written by the late, great Professor George Garratty (Garratty G. How concerned should we be about missing antibodies to low incidence antigens? Transfusion 2003; 43(7): 844-847. DOI: 10.1046/j.1537-2995.2003.00492.x.). SORRY THIS IS A BIT (VERY) LENGTHY!10 points -
This issue - the switch to plastic - seems to bubble up every few years (pardon the minor pun). When I was a puppy in my early years, last century, labs were already tossing around the idea to avoid potentially dangerous, sharp glass tubes. When broken, the plastic used for test tubes is also sharp, possibly worse that glass, as Malcolm suggests. As others have mentioned, static is always an issue with the plastic version, rather than occasional with glass. Other than that, and in my experience, plastic test tubes tubes work almost as well as glass for serological testing. However, many "tube reagents" are not formulated for, or qualified in plastic. The Directions for Use/ Package Inserts may be restrictive. Two points - personal opinion of a cranky old man: 1. One event does not indicate a trend - changing the whole system to address a single cut-finger incident is unreasonable. 2. The various safety apparatuses (however they be mis- or confusingly named) exist to limit institutional legal liability, i.e., prevention of legal action ("please don't sue us"). The workers' actual safety is often secondary.10 points
-
Ah, inform them that by their logic; phlebotomist's should not use needles due to the many unintended sticks in hospitals each year10 points
-

Does anyone knows what does “+s” mean?
Walter Isenheim and 9 others reacted to Malcolm Needs for a topic
It simply means that the P1 antigen is particularly strongly expressed on these red cell samples. Therefore, if you come across a weak anti-P1, it may apparently react with these particular red cell samples, whilst apparently not with, for example, the third red cell sample shown in your antigram. Although not identical to dosage, per se, it is fairly synonymous with dosage at a phenotypical level. The strength of the expression of the P1 antigen is an inherited trait.10 points -
I just saw this seminar being offered by Bio-Rad with our own, infamous, Malcolm Needs as the presenter. I registered and thought I'd pass the word to all of us here. Here is the link:https://info.bio-rad.com/ww-IHD-transfusion-w-registration-lp2.html?elq_mid=48765&elq_cid=10201434&elqCampaignId=30837&utm_campaign=30837&utm_source=eloquaEmail&utm_medium=email&utm_content=Email 13ER EM-R-CM-385201-FY21-TCHS-AWEN_BR-JRNL-TRF News 19 Nov&elqTrackId=6ecbbea5f2bb46849981687404578a8e&elq=7c5f74470efa434dbd4351e512f7ae7a&elqaid=48765&elqat=1&elqCampaignId=3083710 points
-

CPDA-1 Blood
Judes and 8 others reacted to Neil Blumberg for a topic
Our Red Cross just informed us that it will discontinue providing CPDA-1 rbc. We primarily used it to provide volume reduced red cells to pediatric patients under 3 years of age. We will volume reduce AS-1 or AS-3 by centrifugation or washing (Terumo 2991) instead. Probably unnecessary for most patients, but this is a long standing practice here, and it doesn't seem worthwhile trying to adjust pediatric practice in this regard. Most patients do not need the additional volume provided by the anticoagulant-preservative in AS-1, etc., and avoiding unnecessary volume is a reasonable goal in many patients. There is no inherent virtue to CPDA-1 vs. AS-1 and similar solutions, and rbc preservation is slightly better in AS-1/AS-3 by in vitro metrics. There is absolutely no factual basis for using CPD-A1 in preference to AS-1, etc. in pediatrics. Purely expert opinion and probably unduly conservative. I've attached a nice presentation by Dr. Saifee at the University of Washington, who createdAdditive solution AS-1 in Children Univ. Washington presentation Dec 2021.pptx it to educate her colleagues about using AS-1 instead of CPDA-1. Additive solution AS-1 in Children Univ. Washington presentation Dec 2021.pptx Pediatric RBC White Paper - November 2021.pdf9 points -

Confirm anti-D (vs anti-G) via titers?
SbbPerson and 8 others reacted to Malcolm Needs for a topic
It is usual for the C+, D- red cells (e.g. r'r) to react with an anti-G more strongly than a C-, D+ red cell (e.g. R2R2), BUT, this is by no means "diagnostic". As Jsbneg says above, it would be far safer to perform the proper tests, to ensure you have ascertained the correct specificity/specificities. The attached PowerPoint may or may not help (ignore if it is not helpful). The G Antigen and Anti G.pptx9 points -

MTP cut-off policy, or Lethal Dose of Blood Products
Mabel Adams and 8 others reacted to Neil Blumberg for a topic
There are no data suggesting a particular limit. Survival is very unusual after 30-50 units of red cells, but everyone has exceptional cases like those mentioned above. We have discussed futility of care many times, and our practitioners are quite amenable and forthcoming. We have stopped resuscitation in a young man having a liver transplant go badly, when there was no surgical path to hemostasis after about 250 units, but this is unusual too. Bottom line, a case by case decision as to whether care is futile and/or the patient's needs endanger the well being of other patients needing transfusion. Those are the key issues in each case to my way of thinking.9 points -
I have issued 148 units of products to a guy who was cycle vs car massive haemorrhage - he survived. I have issues 120ish units on an obstetric massive haemorrhage (as well as 20 6-packs on the twins) - all 3 survived. I've issued similar on AAA (with eventual bypass) - survival. I think the key is to use TEG to see whether the clotting is screwed - if they are clotting then keep going... In the grand scheme of things blood is cheap9 points
-

Emergency Neonatal Transfusion in Small Hospitals
saralm88 and 8 others reacted to Neil Blumberg for a topic
There is reason NOT to use the freshest possible units. They may be more toxic than intermediate stored units. This is something that made sense but was almost certainly wrong. See below for the reasoning and published data. We use <21 days as fresh for this reason and avoid <7 days storage for everyone based upon the randomized trial data. BMJ 2019;366:l4968 doi: 10.1136/bmj.l4968 (Published 5 August 2019) Page 1 of 1 Letters Trivella and colleagues present some caveats around the subject of duration of red cell storage and clinical outcomes.1 Studies have been widely interpreted as showing that transfusion is not associated with adverse clinical outcomes. I think this is a serious misinterpretation of the data. In addition to the concerns raised by the authors, another valid hypothesis, which has received little attention, is that very short storage red cells might be more dangerous than medium storage periods (say 7-21 days) and equally dangerous as longer storage red cells (say 28-42 days). An inverted U shaped curve. The evidence for this comes from a meta-analysis finding that “ultra short” storage of red cells was associated with a post-transfusion increase in nosocomial infection.2 Shorter storage red cells have a greater imbalance of oxidation-reduction potential than longer storage red cells in preliminary studies in vitro.3 Red cell storage duration is also a poor predictor of post-transfusion free haemoglobin and heme, putative mediators of toxicity from transfusions.4 5 We need better metrics for predicting red cell transfusion efficacy and toxicity. The simple expedient of fresher red cells is clearly not that metric and might be leading us to transfuse more toxic red cells (very fresh) in the most fragile patients, such as premature newborns. A new approach is clearly called for by the current data. At our centre we define fresh as <21 days of storage, and we generally never transfuse a red cell that has been stored for much less than 7-10 days, for the above reasons as well as logistics of supply. Competing interests: None declared. 1 Trivella M, Stanworth SJ, Brunskill S, Dutton P, Altman DG. Can we be certain that storage duration of transfused red blood cells does not affect patient outcomes?BMJ 2019;365:l2320. 10.1136/bmj.l2320 31186250 2 Alexander PE, Barty R, Fei Y, etal . Transfusion of fresher vs older red blood cells in hospitalized patients: a systematic review and meta-analysis. Blood 2016;127:400-10. 10.1182/blood-2015-09-670950 26626995 3 Schmidt A, Gore E, Cholette JM, etal . Oxidation reduction potential (ORP) is predictive of complications following cardiac surgery in pediatric patients[abstract]. Transfusion 2016;56(Supplement S4):20A-1A. 4 Cholette JM, Pietropaoli AP, Henrichs KF, etal . Elevated free hemoglobin and decreased haptoglobin levels are associated with adverse clinical outcomes, unfavorable physiologic measures, and altered inflammatory markers in pediatric cardiac surgery patients. Transfusion 2018;58:1631-9. 10.1111/trf.14601 29603246 5 Pietropaoli AP, Henrichs KF, Cholette JM, etal . Total plasma heme concentration increases after red blood cell transfusion and predicts mortality in critically ill medical patients. Transfusion 2019;59:2007-15. 10.1111/trf.15218 30811035 Published by the BMJ Publishing Group Limited. For permission to use (where not already granted under a licence) please go to http://group.bmj.com/group/rights-licensing/ permissions LETTERS9 points -

Emergency Neonatal Transfusion in Small Hospitals
applejw and 8 others reacted to Neil Blumberg for a topic
If the unit if leukoreduced, as all red cell transfusions should be, there is no need for CMV negative in my view.9 points -

What does Lui stand for? (Freeze-thaw elution)
Walter Isenheim and 8 others reacted to Arno for a topic
In this paper from 1985, "The Lui elution technique A simple and efficient method for eluting ABO antibodies c. s. FENG, K. c. KIRKLEY, c. A. EICHER, AND D. s. DE JONGH, TRANSFUSION 1985; 25:433-434.", the authors thank A. Lui. MT(ASCP)SBB, who introduced this technique to them. Therefore, I believe Lui is the name of the MT who invented this elution method.9 points -

Can I get your opinion or insight on this? Thank you.
Walter Isenheim and 8 others reacted to Malcolm Needs for a topic
In terms of the function of the various ABO blood types, there have been a huge number of peer-reviewed papers written on the subject (and the number has exploded with the advent of COVID19). I would seriously defy anyone to keep up with all of these, but I would recommend reading pages 42-43 of Reid ME, Lomas-Francis C, Olsson ML. The Blood Group Antigen FactsBook. 3rd edition, 2012. Academic Press. ISBN: 978-0-12-415849-8. In terms of how they evolved, it is so far back now that it is anyone's guess, but slides 28 to 32 of the attached lecture may give you some idea. In Depth Lecture on The ABO and H Blood Group Systems.pptx9 points -

Micro only reactions
jojo808 and 8 others reacted to Malcolm Needs for a topic
I have never understood this obsession with looking at reactions down a microscope in blood bank, except looking at things like a Kleihauer or when teaching, to show mixed-field reactions. The great Peter Issitt, not a bad roll model to have, wrote, many years ago now, a passage that I attach from page 69 of his "Applied Blood Group Serology" book, 3rd edition, 1985, Montgomery Scientific Press. That having been said, all reactions seen MUST be recorded, it is just that macroscopic reading is almost all that is ever required.9 points -

Blood Bank Lead - Any advice, tips, ?
DPruden and 8 others reacted to John C. Staley for a topic
Ok, here we go. First is from a personnel stand point. When promoted from with in you are no longer "one of the guys". This means that some of the staff will try to leverage your close friendship which in turn will cause problems with others. Both you and the rest of the staff need to recognize that things have changed on a personal level, at least in the work place. This does not have to be dramatic and should not be, but it is real. Some can do this and some find it very difficult. Now, when coming from outside your are exactly that, an outsider. Now the level of this can vary immensely depending on the situation. One time when I changed facilities it was just across town and I new many of the staff at the new facility so a lot of the unknowns were minimized. On the other hand, I also moved to another facility out of state and pretty much walked into an unknown from a staffing standpoint except for what little I could glean from the interview. As I noted in my previous post, be very judicious when using the phrase, "this is how we did it." I've had new employees who would say this at every opportunity and then go into detail about how we were either doing it wrong and that their way was just much better. This became very trying to everyone else on the staff and we finally just tuned them out. Because of that we probably did miss out on some good ideas. One last point, in either case be aware of any others staff who may have either applied for the position or simply been over looked. Depending on their personality they can either be a great help or a significant hinderance. Do everything you can to get them involved and engaged. They can be your greatest asset but it may take a little extra work on your part. For me, the personnel issues were always the most difficult. I'm assuming that you are new to the lead position and not knowing your previous experience here a couple of generalizations. Unless something is an obvious hazard to either patients, staff or the ability to pass an impending inspection/assessment don't be in a big hurry to make changes. As they say in the military, you need to understand the lay of the land. Become familiar with the blood bank/transfusion service medical director and let them have the chance to become familiar with and confident in you. They can and should be your greatest allies. Ultimately most of what you want to change will have to be approved by them. You need to understand the current processes before trying to change them. At one of the facilities I moved to I noticed that many of the staff were not following their procedures "to the letter". The way I dealt with this was at the monthly staff meeting we would go through a procedure as a group, line by line and I would ask the questions, "Is this how you are really doing it? If not, why not and how are you actually doing it?" This is when I would make suggestions for changes and generally a lively discussion would ensue. It took quite awhile to go through the procedure manual but by picking, what I considered the most important one first it was time well spent. This is getting a little long so I'll end with how I described my position as Transfusion Service Supervisor at a 350 bed level ll trauma center. My job was to provide the staff with the tools (equipment, knowledge, material and support) for them to do their jobs at the highest level possible. All this while keeping the dragons (administration) away from the door. Good luck and if I can think and anything else that others may miss I share a few more golden nuggets of wisdom with you. Above all else have faith in your self. Wow I think that's the longest post I've ever made.9 points -
I would pull the unit from inventory and contact the supplier. They should have the resources to investigate the problem with the donor.9 points
-

Kell & Antibody screening
Walter Isenheim and 8 others reacted to Malcolm Needs for a topic
PLEASE do not worry. Your midwife is COMPLETELY wrong, and really should not comment about something she patently does NOT understand, and about which she has a pitiful amount of knowledge. She should never have answered your questions with her lack of knowledge, but should have left it to your Obstetrician. I note that you are a fellow "Brit"! Within the British population, the percentage of people who have the R1R1 type (which is a type within the Rh Blood Group System) is 16%. Also within the British population, the K- type (which is part of the Kell Blood Group System) is 91%. What that means is that 91% of 16% of the British population is R1R1, K-, or, give or take, a few decimal points, 15% of the British population (about an eighth of the British population). On Friday, 19th October 2018, the British population was measured as 66,690,116! Let's call that 16.5 million in round numbers. This means that, give or take, 9, 975, 000 in Britain are R1R1, K-. Now, admittedly, your midwife will only be looking after women, but, even then, that means 4, 987, 500 women will have the same Rh type and K type as you! How your midwife has only come across your "rare" type four other times in her career, is beyond belief (and I genuinely mean BEYOND belief), unless, as I say, her knowledge of blood groups and blood group serology is incredibly poor, and I repeat, she should NEVER have worried you like this. Just in case you think that I do not know what I am talking about, I have worked in the field of blood transfusion/blood group serology for 43 years, have been an internationally invited lecturer and am the Chief Examiner in Transfusion Science for the Institute of Biomedical Science in the UK, and am a co-author of the British Society of Haematology's Guidelines for Blood Grouping and Antibody Testing in Pregnancy. I don't write that to "blow my own trumpet", as it were, but to try to reassure you that I actually do know what I am talking about. I should warn you that "consulting Dr Google" is equally as useless as listening to your midwife. You should really relax. YES, it is possible for you to produce red cell antibodies during your first pregnancy, but it is INCREDIBLY RARE. It is even more rare for such an antibody to cause any problems in a first pregnancy. I notice that the report from the Blood Bank was that they detected WEAK reactions with 26 of 30 panel cells, but they could not identify a specificity. They have requested three further samples of blood to send to the Reference Laboratory. Again, to give you some comfort, I hope, I ran a Reference Laboratory in London for 16 years before I retired in 2016, and we saw, quite literally hundreds of cases like yours. For a red cell antibody to cause any problems within you pregnancy, it would have to have a titre of 32 or above (this means that it would still be detectable when it has been diluted THIRTY TWO times). I can assure you that the mere fact that the Blood Bank reports weak reactions means that there is ZERO chance that the titre will be 32 or above. If a Hospital Blood Bank, however big or famous the hospital may be, cannot identify an antibody, it is almost universal practice that samples will be sent to a Reference Laboratory for further testing - AGAIN, DO NOT WORRY ABOUT THIS. There are many, many red cell antibodies that are clinically insignificant, both in terms of transfusion reactions and haemolytic disease of the foetus and newborn (which is what your midwife has left you worried about). I KNOW it is difficult, but PLEASE do not worry. PLEASE take no notice whatsoever of your midwife on this matter (I am sure she is an excellent midwife, but she is patently no expert in the field of blood groups), but DO talk to your Obstetrician, who, I hope, will have talked to your hospital's Haematology Consultant, who, in turn, will have spoken to the Consultant in Charge of the Reference Laboratory, and I am sure that they will echo my opinion that there is NOTHING to worry about. Oh, and lastly, I am R1R1, K- myself!!!!!!!!!!!!!9 points -
LOL! We would send it to our reference lab! We have other things to do here... Scott9 points
-

CAP ALL COMMON CHECKLIST COM.04250
SBBSue and 7 others reacted to Malcolm Needs for a topic
So, this PROVES that CAP do not know the A from their elbow. ALL Blood Transfusion Reference Laboratory Staff, not to mention MOST Blood Transfusion Hospital Laboratory Staff KNOW that not all antibodies can, by any means, be detected by ALL serological techniques (saline, albumin, enzyme, LISS, IAT, inhibition tests, recombinant blood group proteins, etc), let alone by ALL technologies (glass, tube, plastic tube, liquid phase microtitre plates, solid phase microtitre plates, column technologies, etc), BUT THOSE WHO RUN CAP KNOW BETTER THAN EVERYONE. They should be thoroughly ashamed of themselves, and go back to kindergarten.8 points -

Antigen typing during pregnancy
Ensis01 and 7 others reacted to John C. Staley for a topic
I've never heard of that. While I can understand the rationale, I'm afraid that if there was enough of a fetal bleed to impact antigen testing mom there are bigger problems than just getting the antigen type right. Just my thoughts.8 points -

Repeat of donor Antigen typing
David Saikin and 7 others reacted to NicolePCanada for a topic
We don't recheck antigen typings here in our hospital in Canada. The typings that have been performed at Canadian Blood Services, are embedded in the barcode on the bag, with all negatives printed on the End User Label. Every unit is antigen typed for K so if it isn't printed on the bag the unit is K Pos. Antigen typings we do are all linked to the unit through barcode. The reason of, "We were typing a lot of units and may have mixed them up", is not acceptable in a blood bank setting. Go work in a different department if you can't organize yourself. Anyway, there is also a full gel or whatever you use crossmatch at the end of that phenotyping, as long as the antibody is reacting, an anomaly could be discovered there. You have to have a little faith that people before you are doing their job properly, or you can cause yourself a lot of undue stress.8 points -

How often must staff sign policies?
TreeMoss and 7 others reacted to Neil Blumberg for a topic
I realize this is "fighting city hall" but is there a more useless requirement than having everyone review and sign off on procedures that haven't changed one iota? In our laboratory, this is many hundreds of procedures (including the one on how to write a a procedure :). Bureaucratic make work of no value whatever. An unfortunate example of the administrative/legal mindset versus the scientific/clinical mindset in our society. Probably an early small sign of the coming end of our civilization when non-productive work receives such priority. Seriously.8 points -

why 3 months?
Yanxia and 7 others reacted to Malcolm Needs for a topic
The three months was chosen following a paper written by Laine EP, Leger RM, Arndt PA, Calhoun L, Garratty G, Petz LD. (In vitro studies of the impact of transfusion on the detection of alloantibodies after autoadsorption. Transfusion 2000; 40 1384-1387. DOI: 10.1046/j.1537-2995.2000.40111384.x.) that showed that red cells that had been transfused (or entered the circulation via a feto-maternal haemorrhage could adsorb out weak alloantibodies for up to three months in a patient with AIHA. This in vivo adsorption would, of course, also apply to individuals who did not have AIHA, but could lead to a secondary stimulation, leading to a stronger antibody (higher titre and higher concentration per mL of plasma), if the alloantibody was "missed" in the antibody screen and/or cross-match, particularly as it is unlikely that the full phenotype of the transfused (or foetal) red cells would be known.8 points -
We had an over zealous infection control team (made up of 100% nurses) come to our lab last year making the same demand. We told them, in essence, we will not comply because the risk of injury from handling those containers were greater than the risk they were trying to alleviate. Furthermore, the risk of accidently confusing saline with formalin, whose containers look exactly alike, was to high when removing from the cardboard containers. In addition to that, we told them the man hours required to keep up with that would require additional FTE's, which would not be approved. They conceded and we continued on, business as usual. TJC does not really inspect labs that are CAP, AABB, or CLIA certified. Those organizations understand the logistics of the cubes and do not have a problem with it. Most infection control officers are nurses and think from the nursing perspective only.8 points
-
Use of plastic tubes for tube testing
AuntiS and 7 others reacted to Sonya Martinez for a topic
I did check our IFU and they did specifically state to use glass tubes. No more arguments.8 points -

Why irradiate liquid plasma when RBCs for trauma patients aren't irradiated?
MinerJ and 7 others reacted to Neil Blumberg for a topic
The mechanisms of what have been termed TRALI (actually a subset of acute lung injury/acute respiratory distress syndrome) and TACO (actually something very common, congestive heart failure) have been widely misunderstood due to unjustified assumptions/dogma. There are many biologic mediators other than antibodies that can cause lung injury after venous infusion which directly subjects the lung vascular endothelium to these mediators (antibodies, activated cells, lipids, mediators such as sCD40L, DNA/histones). Likewise there are many mediators that can cause or exacerbate cardiac failure after venous infusion (inflammatory mediators, excess volume). Cardiac failure is not just volume overload, but can be caused by fever, inflammatory cytokines and vascular/myocardial muscle dysfunction. The notion that these are distinct entities is also at variance with clinical experience. Many patients have signs of both cardiac failure and pulmonary failure simultaneously. So the definitions and pathophysiology used in reviews and texts are lacking in validity and just plain oversimplified and wrong, in my view. There are compelling data to support these iconoclastic contentions for TRALI, and some for TACO. Most germane (see attachment), when we introduced universal leukoreduction, we saw a sustained 83% drop in reports of TRALI and 50% in TACO over the following years. This suggests that white cells/DNA/histones play a role in causing lung and heart inflammation and dysfunction. This clinical observation was confirmed in animal studies from Denisa Wagner's lab at Harvard demonstrating that neutrophil extracellular traps (NETS) infused intravenously can cause acute lung injury (see attachment). To me these observations are convincing evidence that leukoreduction alters cardiorespiratory injury and failure post-transfusion and represents one of the strongest arguments for universal leukoreduction. Needless to say, this challenge to dogma has been ignored by the transfusion medicine community which continues, at least in the USA, to infuse deadly white cells and their degradation products (free DNA/histones) to patients, one of the great tragedies of the last 20 years in the USA blood bank field. We got this entirely wrong and tens of thousands of patients have probably died unnecessarily due to complications of non-leukoreduced transfusions. ULR TRALI TACO PMC version.pdf NETS and TRALI Wagner 2012.pdf8 points -
Tube Antibody Titers: Yes or No to Enhancement?
Malcolm Needs and 7 others reacted to exlimey for a topic
An excellent discussion point. I think many others have similar questions and concerns. The have been several other threads on this forum with similar subject matter. As an Old Fart, I feel obliged to spout some (un-referenced) history. Most of the original work on clinical significance of antibodies in pregnancies was done in the absence of potentiators and definitely before the use of (semi)automated test systems. I think it was a "saline-IAT" using 22% albumin (BSA) as a diluent. Most of those antibodies were anti-D, for obvious reasons. There's not much out there in the literature in terms of controlled or organized studies regarding other specificities. There are a fair number of one-of-a-kind case studies, but most of the stuff is retrospective analysis of data. Basically, other than anti-D, nobody really knows what an antibody titer means, but as Ensis01 suggests, detecting a change in titer (increase) may be more important. In an era when basic tube shaking is going away, it only makes sense (we have no other option) to convert to the new techniques and equipment, but I suspect that it has the potential to further confuse an issue which already has enough confusion to (dis)satisfy everyone. I don't envy anyone handling this hairball. As a last thought...the high-powered potentiators (and techniques) used today don't reflect what's going on in vivo. Arguably, if one ignored the 22% BSA diluent, the saline-IAT is a better mimic of the in vivo scenario.8 points -
I think we need to add an OMG emoji to our selections!8 points
-

Fellowship of the British Blood Transfusion Society.
Sonya Martinez and 7 others reacted to Malcolm Needs for a topic
8 points -

Antibody stimulation by antigen negative blood?
Walter Isenheim and 7 others reacted to Arno for a topic
Hi Rich, I am not a clinician but as far as I know IVIG can be given to obstetrical patient in diff. conditions (autoimmune disorders, recurrent pregnancy loss, ...). I thought about IVIG when I saw the DAT becoming positive plus additional reactions coming up over the time. Anti-A and Anti-B are indeed the most prevalent antibodies in plasma derived products but other specificities of low titre can be present sometimes such as anti-D, anti-K and a bunch of antibodies of undetermined specificity reacting with several to not say all RBCs. Just a thought that can be doublechecked with the clinician..? Hereunder is a very great (not recent though) paper to be read and re-read again: Problems Associated With Passively Transfused Blood Group Alloantibodies George Garratty, PhD, FRCPath American Journal of Clinical Pathology, Volume 109, Issue 6, 1 June 1998, Pages 769–777, https://doi.org/10.1093/ajcp/109.6.7698 points -

translation of antibody screen result
SbbPerson and 7 others reacted to Malcolm Needs for a topic
Before I attempt to answer your query, I must explain that I am NOT a doctor. I am what is called in the UK, a Biomedical Scientist and, as such, am not qualified to make a diagnosis, but I am the Chief Examiner in Transfusion Science for the Institute of Biomedical Science, and used to by the Reference Laboratory Manager in the Red Cell Reference Laboratory in the National Health Service Blood and Transplant Centre in Tooting, London, so I can claim some expertise. Although a warm auto-antibody in a person's plasma is by no means common, it is something we use to see on a daily basis at Tooting. To put it at its most basic, it results from your immune system producing an antibody directed against a red cell antigen expressed upon your own red cells, which could, under certain circumstances, lead to you becoming (usually mildly) anaemic. The "autologous adsorption" bit means that the laboratory, either at your hospital, or at a Reference Centre has been able to remove the antibody from the plasma in your blood sample by using your own red cells (thus proving beyond doubt that the antibody is indeed an auto-antibody). They have then tested this adsorbed plasma in tests to see if there are any unusual antibodies in your plasma that are directed against antigens expressed on the red cells of other individuals; so called allo-antibodies. They include in their report the caveat that concerning the "common blood group antigens" because it is all but impossible to test for antibodies against all the known antigens, of which there are well over 600, some of which are incredibly rare. Most auto-antibodies have a specificity within the Rh Blood Group System, which, at present, contains 55 different antigens (but other antigens are being found on a regular basis). Most of these auto-antibodies are directed against either the Rh antigen known as Rh17, or against that known as Rh18 (I realise these names will mean nothing to you - but bear with me). Almost everybody in the world expresses both of these antigens on there red cells, and the actual specificity of the auto-antibody is not really of any consequence. It is highly unusual, to say the least, for a maternal auto-antibody to cause any problems with a condition known as haemolytic disease of the foetus and new-born (or HDFN), particularly at an early stage of pregnancy. To me, this suggests that your early miscarriages and your auto-antibody status are coincidental, rather than the auto-antibody being the cause of your early miscarriages. Red cells are not really produced in early foetal life (indeed, there is not much in the way of blood in a foetus until about 12 weeks of gestation), so there are very few foetal red cells available to be affected by your auto-antibody. Having said all of that, I would reiterate that I am NOT a doctor, and even if I were, it would be impossible (and stupid in the extreme) to even attempt to make a diagnosis without FULL knowledge of your case. As such, I would suggest that you do discuss your case with your own physician (or your obstetrician) and be guided by what he or she suggests in terms of further testing. I hope that helps a little bit, and that I have not "blinded you with science" (which was not my intention), and I apologise for me English spelling!8 points -

Neil Blumberg
TreeMoss and 7 others reacted to Neil Blumberg for a topic
And to give credit where credit is due, whatever I have achieved has been with the invaluable contributions of my collaborators, including physicians, scientists, medical technologists and nurses. In particular, my most important collaborator has been my wife, Dr. Joanna Heal MBBS, MRCP, whose brilliance and dedication to patient care made all the difference. That's her in the picture :).8 points -

Kell & Antibody screening
Walter Isenheim and 7 others reacted to Malcolm Needs for a topic
Thanks ELondon. Could I just say again, even if the Reference Laboratory does detect an antibody (or more than one, come to that), it is not a particularly abnormal thing in pregnancy, but it does not mean for one minute that the pregnancy will be affected; Mother Nature has seen to that. There is another Blood Group System named Lewis. The antigens within this system are soluble in the plasma part of your blood, and are adsorbed onto the red cells from the plasma (they are not intrinsic to the red cell membrane). During pregnancy, the concentration of plasma lipoproteins (fatty proteins in the plasma) can increase enormously (about four-fold). These plasma lipoproteins "mop up" the soluble Lewis antigens, and a pregnant woman, who would normally be, for example, Le(a-b+), can become Le(a-b-), and may even, temporarily, produce antibodies against the Lewis antigens (an individual hardly ever produces antibodies against an antigen that they express - but strange things happen in pregnancy!). In addition, ALL babies are born as Le(a-b-), so any Lewis antigens Mum produces will NOT affect the baby! There are many, many other antibody specificities that will not affect the pregnancy at all. Now, I should say two things. Firstly, I cannot say, from a distance, what is the antibody in your plasma (that can only be done by the laboratories at the Hospital and the Reference Laboratory, but it does not sound at all serious). Secondly, i am what is called a Biomedical Scientist, not a doctor, and so I am, by Law, not allowed to diagnose (as far as I know, neither is the midwife), and this is why I am so glad that you are going to see an Obstetrician, who, I hope, will be able to reassure you even more. Mean while, sleep easier, and enjoy your pregnancy!8 points -

How not to miss a weak reaction
Kelly Guenthner and 6 others reacted to Malcolm Needs for a topic
It sounds to me like you are doing everything that you should do, without either over-shaking the tube, or over-reading the contents. I am extremely glad that you are not using a microscope, as, if you did, you would almost certainly see the odd couple of red cells "kissing each other", even if they have been incubated in isotonic saline. The other thing is (and I speak with some 43 years of working in blood group serology) if the reactions in the tube are THAT weak, the chances of any atypical alloantibody that you might miss being clinically significant are absolutely minute. If you are still worried, however, get a more experienced worker to read your tests as well, until you feel confident. That is how I learned when I started. I wish you the best of luck in your future career.7 points -

Platelet Compatibility
CARMEN DELGADO and 6 others reacted to Neil Blumberg for a topic
Another point. Since group O whole blood has proven as safe or even safer than typical component therapy (A platelets, A or AB plasma) in massive transfusion of trauma patients, perhaps group O low titer platelets would be safer than group A or B platelets for an AB patient :)? No one knows, but worth considering. The big problem is probably giving non-O platelets to O patients. There is evidence this increases bleeding and mortality. Just like red cells, only O platelets for O recipients is a good practice. The AB patient may be less of a problem, since giving some small amount of antibody may be less dangerous. A risk of hemolytic reaction of about 1 in 700 or so. The risk of mortality in transfusing an O patient with A platelets is probably 1 in 5 (see attached). ABO incompatible platelets intracranial bleeding 2021.pdf ABO plasma incompatible platelets and hemolytic reactions.pdf7 points -

Platelet Compatibility
TreeMoss and 6 others reacted to Neil Blumberg for a topic
"Since AB+ people are considered the "universal recipient" , we give them any type platelets, usually starting with the one with the closest out date. " I grant you that this is widely shared idea in our field for decades. It is also seriously wrong. It prioritizes inventory management over patient wellbeing. Our approach to ABO and platelets is distinctly different from ABO and red cells with no rational basis. Antibody and complement destroy red cells and platelets equally well. The only difference is that instead of free hemoglobin being released, it's mediators such as VEGF, IL-6 and other platelet pro-inflammatory, immunomodulatory and pro-thrombotic granule contents are released. ABO mismatched platelet transfusions at least double the refractoriness rate in repetitively transfused patients (see attached for references), and actually increase bleeding and mortality. The answer to the question is ABO identical is by far most effective and safest. If you have to give ABO mismatched, there is probably no good answer other than washed/volume depleted O's, A's or B's, where most of the incompatible plasma is removed. If that's not possible, postponing platelet transfusion until ABO identical is available when feasible, giving half doses of ABO identical if two patients need the one available unit, etc. are also reasonable. Sadly, ABO mismatched platelets are probably worse than no platelets at all. They provide little or no hemostatic benefit and increased risks of bleeding, organ injury and death for the patient. If I were the attending physician, I would generally give no platelets if ABO identical or washed O's weren't available in a stable, non-bleeding patient with a count of over 5,000. The good news is we can improve outcomes by just doing what we do for red cells. Do not transfuse ABO incompatible antigen or antibody. It's bad for red cells, platelets and endothelial cells, all of which have complement and Fc receptors that bind immune complexes, and all of which bear ABO antigens on their surfaces. Carr ABO mismatched refractoriness copy.pdf ABO story expanded.docx ABO endothelial cell paper.docx NEJMc2034764 copy.pdf NEJMc2034764_appendix copy.pdf7 points -
Here is an interesting paper showing that antibodies to red cell/platelet... may be transmitted via breast milk indeed, causing prolonged HDFN. Milk contains mostly IgA but IgM and IgG may be present of course and IgGs can cross the different barriers up to blood circulation (not on the same model - not actively - as the placenta though). The surprizing part here is the mother and baby are group A, A antigen is ubiquitous so the anti-A titer in breast milk should high enough to interfer with reverse group despite the adsorption of anti-A on various tissues. https://pubmed.ncbi.nlm.nih.gov/30720868/7 points
-

Patient with WAA unable to determine ABO & Rh type
applejw and 6 others reacted to Malcolm Needs for a topic
With all due respect, if you do not trust the results given to you by your IRL, why did you send samples to them in the first place? The other thing is that the term "least incompatible" has been "rubbished" by LaTwrie Petz almost 20 years ago now (and you can't get much better than him!) - see Petz LD. "Least incompatible" units for transfusion in autoimmune hemolytic anemia: should we eliminate this meaningless term? A commentary for clinicians and transfusion medicine professionals. Transfusion 2003; 43(11): 1503-1507. DOI: 10/1046/j.1537-2995.2003.00583.x. I apologise if this reads as I am being personally rude to you; that is DEFINITELY NOT my intention.7 points -

What is the meaning of this?
Yanxia and 6 others reacted to Malcolm Needs for a topic
What you are identifying is almost certainly a strong anti-H in an Oh individual. However, if the individual requires a transfusion, you will need to perform differential allo-adsorption (or something similar) to identify any other underlying clinically significant atypical antibodies (you can ignore any underlying Lewis antibodies, which are commonly also present).7 points



.thumb.jpg.eee1087fb65cc085b02546dca3598a62.jpg)

.thumb.jpg.661aecd95f256d3871848215f4b4930c.jpg)